Similar to people, mice that consume a high-fat diet not only become obese, but also tend to be anxious and depressed. Scientific research backs up this observation as it has found that obesity and mental disorders such as depression and anxiety seem to often go hand in hand.

At Baylor College of Medicine Dr. Qi Wu and his colleagues at collaborating institutions are providing new insights into this association. They have identified and characterized a novel neural circuit that mediates the reciprocal control of feeding and psychological states in mouse models.
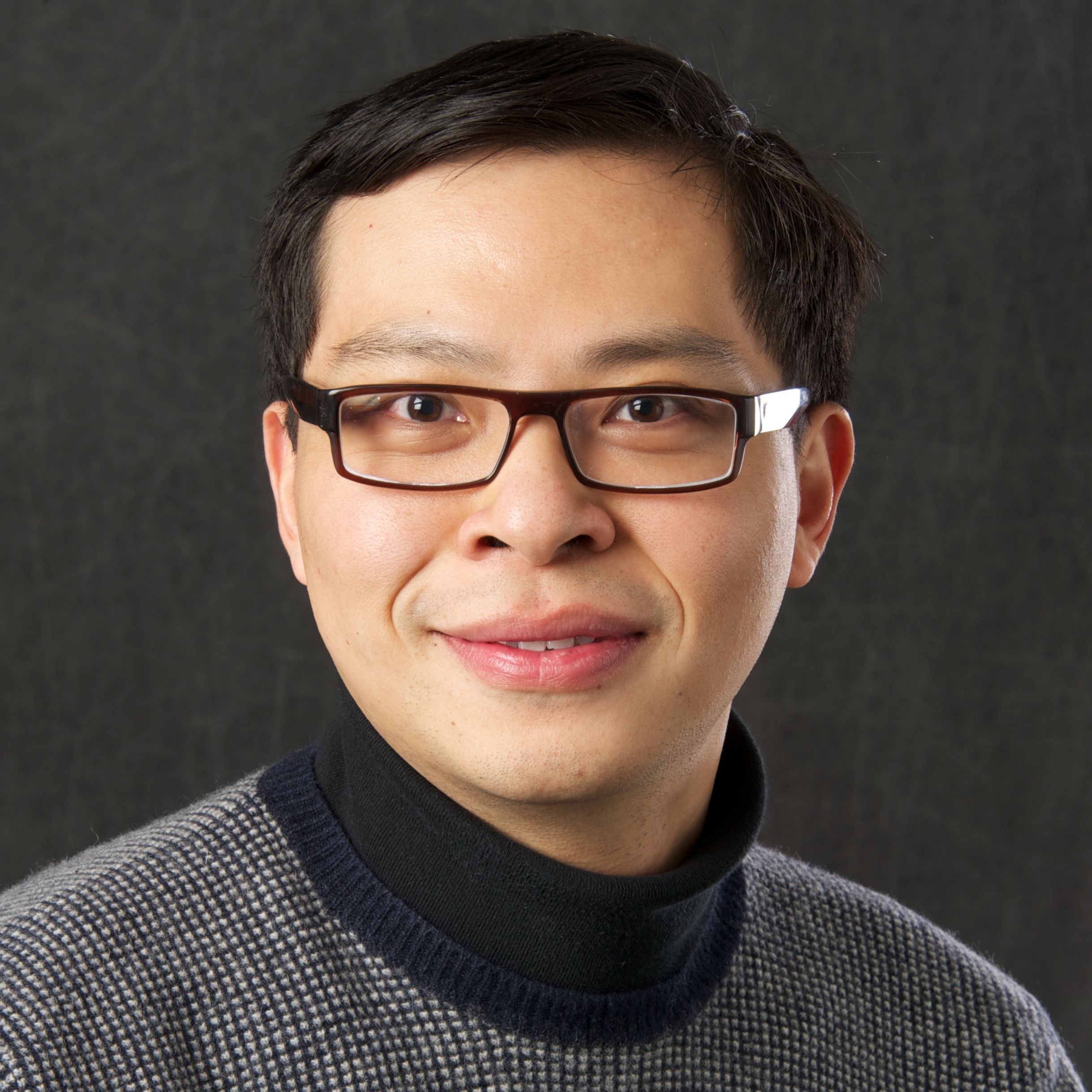
“Reports indicate that 43% of adults with depression are obese and that adults with mental illness are more likely to develop obesity than those who are mentally healthy,” said Wu, a Pew Scholar for Biomedical Sciences, Kavli Scholar and assistant professor in pediatrics-nutrition at Baylor’s Children’s Nutrition Research Center. “Factors such as hormonal dysregulation, genetic deficiency and inflammation have been proposed to be involved in the connection between obesity and mental disorders. Here we provide evidence that supports the involvement of a neural component.”
A novel brain circuit connects obesity and depression
To investigate the neuronal circuits that could be involved in reciprocally regulating weight gain and depression or anxiety, the researchers provided mice with a high-fat diet. As expected, the animals became obese. They also developed anxiety and depression. In these mice, the team studied the function of neuronal circuits.
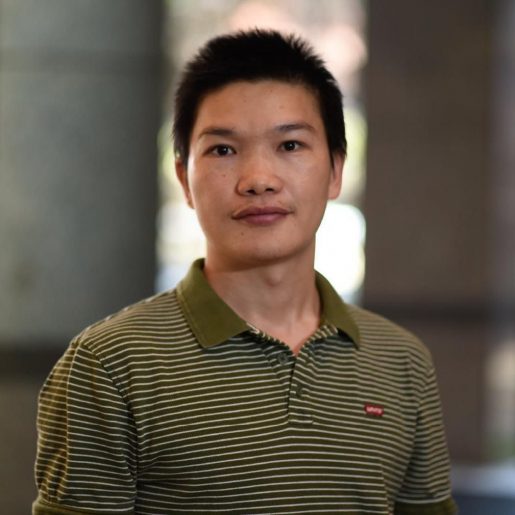

“We discovered in normal mice that two groups of brain cells, dBNST and AgRP neurons located in separate brain areas, form a circuit or connect to each other by extending cellular projections,” said co-first author Dr. Guobin Xia, postdoctoral associate in the Wu lab. “This newly discovered circuit was malfunctioning in mice that were both obese and depressed.”
“Using genetic approaches, we identified specific genes and other mediators that were altered and mediated the circuit’s malfunction in the obese and depressed mice,” said co-first author Dr. Yong Han, postdoctoral associate in the Wu lab.
Repairing the defective brain circuit changed the animals’ food preferences
“Importantly, genetically restoring the neural defects to normal eliminated the high fat diet-induced anxiety and depression and also reduced body weight,” Xia said. “We were surprised to see that the animals lost weight, not because they lost their appetite, but because genetically-aided readjustment of the mental states changed their feeding preferences.”
Before the treatment, the mice naturally preferred to eat a high-fat diet, but after the treatment they preferred a healthier diet with reduced fat and abundant protein and carbohydrates.”
Keeping in mind potential translational applications of their findings to the clinic, Wu and his colleagues investigated the possibility of restoring the novel circuit pharmacologically.
“We discovered that the combination of two clinically-approved drugs, zonisamide and granisetron, profoundly reduced anxiety and depression in mice and promoted weight loss by synergistically acting upon two different molecular targets within our newly identified brain circuit,” Wu said. “We consider that our results provide convincing support for further studies and future clinical trials testing the value of a cocktail therapy combining zonisamide and granisetron (or a selection of their derivatives) to treat metabolic-psychiatric diseases.”
For the first time, these findings not only reveal a key regulatory mechanism for coinciding obesity and mental disorders, but also suggest the possibility of a pharmacological treatment.
Read the complete report in the journal Molecular Psychiatry.
Other contributors to this work include Fantao Meng, Yanlin He, Dollada Srisai, Monica Farias, Minghao Dang, Richard D. Palmiter and Yong Xu. The authors are affiliated with one of the following institutions: Baylor College of Medicine, Vanderbilt University School of Medicine, University of Texas MD Anderson Cancer Center and University of Washington, Seattle.
This work was supported by NIH grants (1R01DK109194, 1R56DK109194, R01DK093587, R01DK101379, R01DK117281, and R01-DA24908), Pew Charitable Trust awards, American Diabetes Association awards (7-694 13-JF-61, 1-17-700 PDF-138), American Heart Association awards (17GRNT32960003), USDA/CRIS grants (3092-5-001-059), Baylor Collaborative Faculty Research Investment Program grants and Faculty Start-up grants from USDA/ARS. Further support was provided in part by NIH Centers of Biomedical Research Excellence, COBRE grant (P20 GM135002), IDDRC Grant Number U54HD083092 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development, the Clinical and Translational Proteomics Service Center at the University of Texas Health Science and the Howard Hughes Medical Institute.
