Source/Disclosures
Disclosures:
Khanna reports receiving consulting fees from Edwards Lifesciences, Medtronic and Philips North America, and grant support from the NIH/National Center for Advancing Translational Sciences Wake Forest Clinical and Translational Science Institute for a randomized trial of continuous postoperative hemodynamic and respiratory monitoring. Please see the study for all other authors’ relevant financial disclosures.
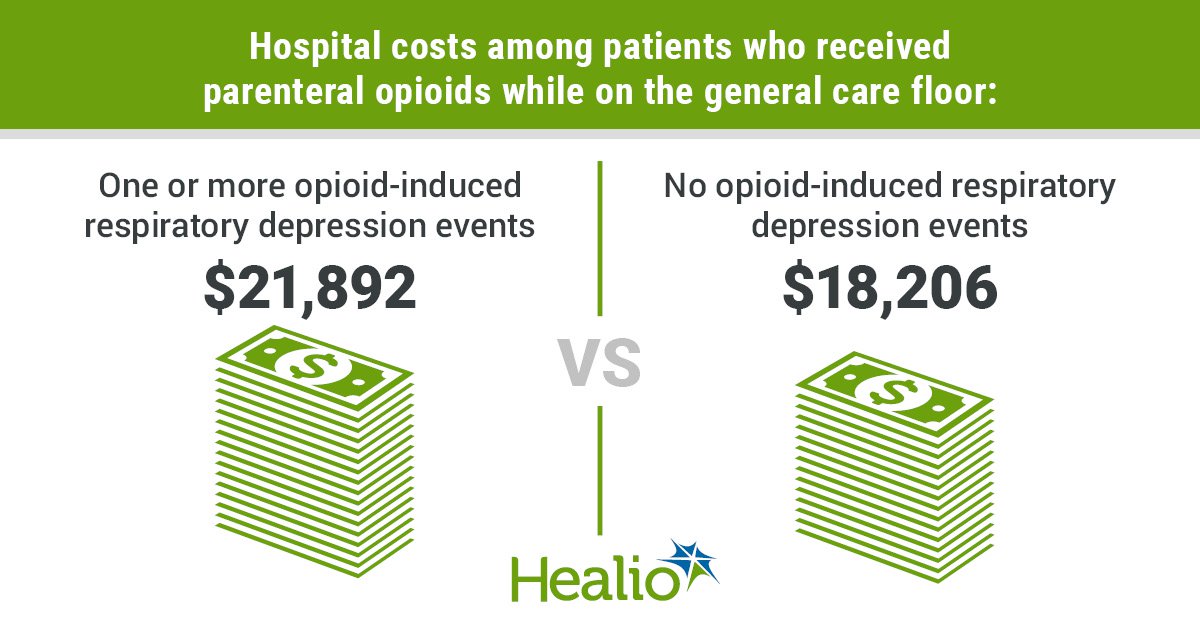
Researchers reported that patients who experienced at least one opioid-induced respiratory depression event on a hospital’s general care floor spent about 6 days in the hospital and had more than $21,000 in related costs.
These numbers are significantly higher than the average length of hospital stay and related costs among patients who did not have an opioid-induced respiratory episode on a hospital’s general care, the researchers added.
Reference: Khanna et al. BMC Anesthesiol. 2021;doi: 10.1186/s12871-021-01307-8.
While this “is a very obvious fact, the magnitude of these outcomes is very disturbing and surprising,” Ashish Kumar Khanna, MD, FCCP, FCCM, study author and an associate professor of anesthesiology at the Wake Forest University School of Medicine, told Healio Primary Care.

Ashish Kumar Khanna
Khanna and colleagues previously published data from the PRODIGY trial, where nearly half of 1,495 inpatients aged 18 years and older from 16 sites across seven countries experienced an opioid-induced respiratory depression event, which was detected through nonstop oximetry and capnography monitoring.
“A natural next question was to access the relationship of opioid-induced respiratory depression on health care resource utilization, and costs associated with adverse events linked to this as we recover patients in the hospital,” Khanna said.
The researchers assessed the relationship between opioid-induced respiratory depression and health care resource utilization in 1,335 adults (including 769 from the United States) from the PRODIGY trial. The patients were given parenteral opioids and underwent uninterrupted capnography and pulse oximetry monitoring. Khanna and colleagues retrospectively collected data on hospital costs for 420 U.S. patients.
The researchers reported that inpatients with one or more opioid-induced respiratory depression events had a longer length of stay (6.4 vs. 5 days; P = .009) and higher hospital costs ($21,892 vs. $18,206; P = 0.002) compared with patients who did not have an episode. Also, inpatients who had high PRODIGY respiratory depression risk scores and one or more opioid-induced respiratory depression events had higher hospital costs compared with high-risk patients who did not have an episode ($21,948 vs. $18,474, P = .0495). A propensity weighted analysis revealed that inpatients with one or more opioid-induced respiratory depression events had 17% higher costs than those who did not (P = 0.007).
Khanna and colleagues noted that the results draw attention to “the unmet need in the quality of care for general care floor patients receiving opioids.”
“Opioid induced respiratory depression is common and prevalent on hospital general care floors,” Khanna said. “Early identification of patients at risk for respiratory depression, along with early proactive intervention, may reduce the incidence of respiratory depression and its associated clinical and economic burden.”
The next steps of this research “will be to perform a true cost-effectiveness analysis and build a model which will allow clinicians and hospital administrators to calculate a ‘break-even’ point for investment into increased continuous surveillance monitoring tools and how much of a decrease in opioid induced respiratory depression would allow for a break-even investment point,” Khanna said.


