Source/Disclosures
Disclosures:
Musliner reports receiving grants from the Lundbeck Foundation during the conduct of the study. One study author reports receiving grants from the Danish Cancer Society, the Independent Research Fund Denmark, the Lundbeck Foundation and the Novo Nordisk Foundation during the conduct of the study. The other authors report no relevant financial disclosures.
Higher polygenic liability for major depression was linked to increased risk for recurrent depressive episodes, according to results of a population-based cohort study in a research letter published in JAMA Psychiatry.
“To our knowledge, no study has examined whether polygenic risk scores (PRSs) can prospectively predict recurrence among individuals with first-onset depression,” Katherine L. Musliner, MPH, PhD, of the National Centre for Register-based Research, at Aarhus University in Denmark, and colleagues wrote. “Furthermore, to our knowledge, no study has evaluated whether PRS could potentially be useful for predicting recurrence in a clinical setting. Therefore, our goal was to examine whether higher PRS for [major depression] (PRS-MD) was associated with increased risk [for] recurrence in individuals diagnosed with unipolar depression in hospital-based settings and to estimate the absolute risk [for] recurrence based on polygenic risk.”
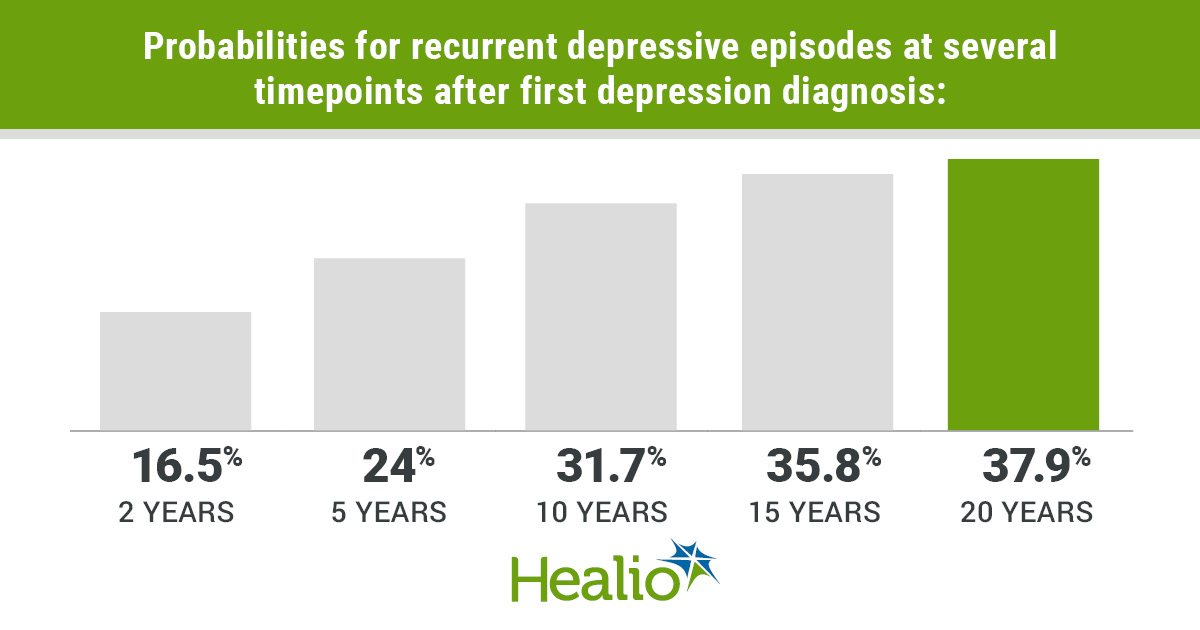
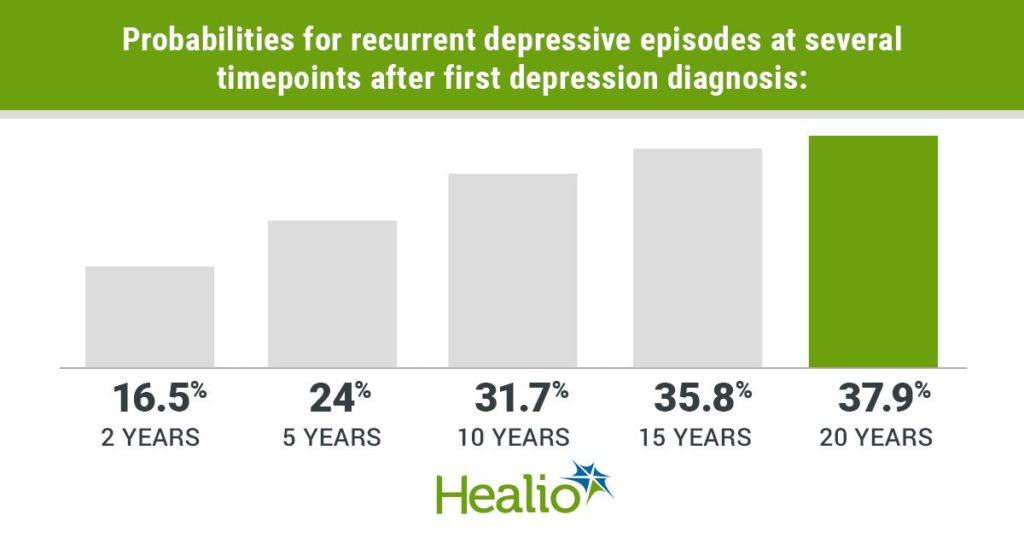
Infographic data derived from: Musliner KL, et al. JAMA Psychiatry. 2021;doi:10.1001/jamapsychiatry.2021.0701.
The researchers also aimed to evaluate the specificity of the link between PRS-MD and recurrence by assessing whether there were associations between increased risk for recurrence and PRS for bipolar disorder (PRS-BD), schizophrenia (PRS-SZ) and ADD (PRS-AD). They obtained data from a case-cohort sample of 16,180 individuals (mean age at first depression diagnoses, 19.1 years; 68.3% women) diagnosed with a single depressive episode according to ICD-10 criteria who had no prior bipolar or schizophrenia spectrum diagnoses and were aged 10 to 32 years in publicly fund psychiatric hospital inpatient, outpatient or ED settings in Denmark between Jan. 1, 1995, and Dec. 31, 2016. The researchers considered a subsequent depression diagnosis a recurrent episode if it occurred 8 weeks or longer after the end date of the first contact, which meant follow-up began 57 days following the end of the first depression episode and ended at the second depression episode’s date of contact, death, emigration or Dec. 31, 2016, whichever came first.
Results showed a range of 2 months to 17 years for time to recurrence among individuals who had a recurrent episode. The researchers noted that at 2, 5, 10, 15 and 20 years after the first diagnosis of depression, probabilities of recurrence were 16.5% (95% CI, 15.9-17), 24% (95% CI, 23.4-24.7), 31.7% (95% CI, 30.9-32.6), 35.8% (95% CI, 34.5-37.1) and 37.9% (95% CI, 35.1-40.8), respectively. Musliner and colleagues reported that PRS-MD exhibited a significant association with recurrence risk, which remained after they controlled for the other PRSs and had an adjusted HR ratio per one-SD increase of 1.07 (95% CI, 1.04-1.1). The other PRSs were not linked to recurrence. Individuals with PRS-MD two SDs below the mean after 20 years exhibited a 34.4% (95% CI, 31.4-37.6) risk for recurrence; those with two SDs above the mean exhibited a 41.6% (95% CI, 38.2-45.2) risk for recurrence.
“These results are consistent with prior studies and lend support to the hypothesis that individuals with recurrent depression may have, on average, a higher genetic loading than individuals with a single episode of depression,” Musliner and colleagues wrote. “This association appears to be specific to PRS-MD, as we found no evidence that polygenic liability for other psychiatric disorders was associated with recurrence risk. These results may not be generalizable outside of Denmark or to patients with [major depression] who do not receive hospital-based care.”