1NIMH Clinical Center, National Institute of Mental Health Czech Republic, Klecany, Czech Republic; 2Department of Psychiatry and Medical Psychology, Third Medical Faculty, Charles University, Prague, Czech Republic
Correspondence: Martin Hejzlar
National Institute of Mental Health Czech Republic, Topolova 748, Klecany, 250 67, Czech Republic
Tel +420 283 088 314
Email [email protected]
Background: There are no head-to-head studies comparing the antidepressant effect of transcranial direct current stimulation (tDCS) with repetitive transcranial magnetic stimulation (rTMS). This pooled analysis compared indirectly the antidepressant efficacy and acceptability of rTMS, tDCS, and the antidepressant venlafaxine (VNF) extended-release.
Methods: The analysis (n=117, both patients with treatment-resistant depression (TRD) and non-TRD were included) examined pooled data from two 4-week, single-centered, two-armed, double-blind, randomized studies (EUDRACT n. 2005-000826-22 and EUDRACT n. 2015-001639-19). The antidepressant efficacy of right-sided low-frequency rTMS (n=29) vs VNF (n=31) and left-sided anodal tDCS (n=29) vs VNF (n=28) was evaluated. The primary outcome was a change in the Montgomery–Åsberg Depression Rating Scale (MADRS) score from baseline to the treatment endpoint at week 4. The response was defined as a ≥ 50% reduction in the MADRS score and remission as the MADRS score ≤ 10 points, both were calculated for the primary treatment endpoint at week 4.
Results: Mean change in total MADRS scores from baseline to week 4 was 7.0 (95% CI, 4.8– 9.1) points in the rTMS group, 7.6 (95% CI, 5.5– 9.8) in the tDCS group, and 8.9 (95% CI, 7.4– 10.4) among patients in the VNF group, a non-significant difference (F(2111)=0.62, p=0.54). Similarly, neither the response rates nor remission rates for rTMS (response 31%; remission 17%), tDCS (24%, 17%), or VNF (41%; 27%) significantly differed among treatment groups (χ2=2.59, p=0.28; χ2=1.66, p=0.44). Twenty patients (17%) dropped out of the studies in a similar proportion across groups (rTMS 3/29, tDCS 6/29, VNF 11/59, χ2=1.41, p=0.52).
Conclusion: Our current analysis found a comparable efficacy and acceptability in all three treatment modalities (rTMS, tDCS, and VNF) and clinical relevance for the acute treatment of major depressive disorder.
Keywords: repetitive transcranial magnetic stimulation, rTMS, transcranial direct-current stimulation, tDCS, venlafaxine, major depressive disorder, MDD, treatment, efficacy
Introduction
Major depressive disorder (MDD) is a severe mood disorder often associated with a poor response and recurrent course. Available treatments – pharmacological and non-pharmacological – are continually under investigation, because MDD is one of the leading causes of disability. It also presents a significant economic burden globally.1 According to a recent meta-analysis of the efficacy of antidepressants (ADs), all the ADs analyzed (k=21) were more efficacious than placebo.2 The effectiveness of ADs in MDD treatment – shown by the number needed to treat (NNT) compared to placebo – reached NNT=5.4 for response and NNT=7.3 for remission.3 A new meta-analysis of various ADs used in primary care resulted in comparison via NNT of tricyclics (TCAs)=8.5, serotonin reuptake inhibitors (SSRIs) NNT=6.5, and venlafaxine (VNF) NNT=6.4 However, one-third of patients does not respond to the first AD treatment5 and potential undesired effects of ADs occur frequently.6 There is a clear clinical need for developing other AD treatments and strategies.7
During the past decades, non-invasive brain stimulation (NIBS) methods such as repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS) have been increasingly used and examined. The efficacy of rTMS in the treatment of MDD has been supported by several meta-analyses.8,9 Low-frequency rTMS (LF rTMS, ≤1 Hz) over the right dorsolateral prefrontal cortex (DLPC) and high-frequency rTMS protocols (HF rTMS, ≥5 Hz) over the left DLPC are considered to be of similar effectiveness in the acute treatment of MDD.10,11 LF rTMS reached for both response and remission NNT=5.12 According to the updated Canadian Network for Mood and Anxiety Treatments (CANMAT 2016) clinical guidelines, rTMS was set as a first line neurostimulation treatment for patients after at least one AD had failed.13 The use of tDCS is a relatively new approach in the treatment of MDD. Older meta-analyses have demonstrated mixed results.14–16 The newer ones have shown the superiority of tDCS over sham stimulation, but the clinical usefulness of tDCS in the treatment of MDD remains questionable.17,18 A recent meta-analysis based on individual patient data also confirmed that active tDCS was superior to sham stimulation both in response (NNT=9) and remission rates (NNT=13). The clinical effects of tDCS were described as moderate.19 According to the CANMAT guidelines, tDCS is recommended as a third line treatment for MDD.13
Research on the efficacy of rTMS and tDCS in the treatment of MDD is still in progress. No head-to-head study has compared the antidepressant effect of tDCS and rTMS. There is still a relative paucity of data on the comparison of rTMS and tDCS with each other. In our study, we display an analysis of our original data from two randomized controlled trials (RCTs) with almost identical designs comparing efficacy and tolerability of rTMS, tDCS, and venlafaxine.20,21 Both studies were carried out in one center, on the same department, and by almost the same research team.
Methods
Study Design
The analysis examined pooled data from the two trials mentioned above. Briefly, two 4-week, single-centered, two-armed, double-blind, randomized studies (EUDRACT n. 2005-000826-22 and EUDRACT n. 2015-001639-19) were conducted in Prague Psychiatric Centre (PCP)/National Institute of Mental Health (NIMH-CZ), Czech Republic, between 2005–2009 and 2015–2019.20,21 The design of both studies adhered to the latest version of the Declaration of Helsinki and ICH/Good Clinical Practice guidelines, both trials were regulated by the State Institute for Drug Control of Czech Republic (SUKL). PCP Independent Ethics Committee (IEC) (for the first trial) and NIMH-CZ IEC (for the second trial) reviewed and approved the study and written consent to participate in the research was obtained from all subjects.
Subjects
The current pooled analysis comprised data from the 117 patients who participated in both studies; 84 (72% of the sample) were women. The main inclusion criterion was the diagnosis of MDD (recurrent or single episodes) according to the Diagnostic and Statistical Manual of the American Psychiatric Association, 4th edition22 and the Mini-international neuropsychiatric interview (MINI), Czech version 5.0.0.23 Enrolled patients needed to have the baseline MADRS score >20 points in the rTMS study and >25 points in the tDCS study. As chosen MADRS scores respond to moderate depression (usual cutoff points are 20–34), the slightly higher score in the second trial could ensure more precise enrollment of moderately depressed patients to the study. Other inclusion criteria were age (18-65 years), right-handedness, and no contraindications for tDCS/rTMS treatment. We recruited inpatients from the open ward of PCP/NIMH-CZ. Patients who had not responded to VNF in current or previous episodes were not enrolled in the trials. We excluded patients with suicidal risk, patients who suffered from psychiatric comorbidity on axis I (including anxiety disorders), serious medical unstable illnesses, or neurological disorders (eg, epilepsy, brain injury, and risk of seizures). Pregnant and breastfeeding women were excluded from the study. The complete details on the inclusion and exclusion criteria are available in the original articles.
Treatment Used in the Studies
The first trial evaluated the AD efficacy and acceptability of right-sided LF rTMS vs VNF. The second trial compared left anodal tDCS vs VNF. Following the wash-out period (5–9 days in the rTMS study; 2–7 days in the tDCS study), inpatient participants were randomized either to the active rTMS/tDCS+placebo group or the VNF+sham rTMS/tDCS group. The subjects then received a 4-week treatment. In the first trial, we applied 20 sessions of rTMS (1Hz over the right DLPC, 600 pulses per session, 100% of motor threshold, once a day, n=29). In the second trial, the patients received 20 tDCS stimulation (2 mA, anodal stimulation over the left DLPC, cathode was placed over the right DLPC, 30 minutes, once a day, n=29). The locations of the anode and cathode placement corresponded to F3 and F4 areas according to the 10–20 EEG coordinate system. Patients assigned to the VNF groups (n=59; rTMS study n=31; tDCS study n=28) started the study treatment with 75 mg of venlafaxine per day and took a dose of at least 150 mg per day of VNF from the second week of the treatment. Further dosage titration was scheduled according to the clinical decision of the attending physician. The daily dose of VNF could be increased by 75mg every 5 days to a maximum of 375 mg of VNF per day. The dose could be decreased to 150 mg per day due to safety and tolerability reasons. Patients who did not tolerate at least 150 mg of VNF per day were excluded from the study. The average final doses of VNF in both studies was 246 mg per day (min-max range, 150–375 mg). The application of sham stimulations (tDCS, rTMS) and placebo capsules is described in detail in the original articles.20,21
Clinical Assessment
Assessments were performed by clinical psychiatrists before the wash-out period, at baseline, and weekly up to week 4. The raters were trained according to the criterion of intraclass correlation >0.80 for each clinician before conducting ratings. The primary endpoint was a change in the MADRS score from baseline to week 4.24 The secondary outcomes were as follows: a change in MADRS score on a visit-by-visit basis; response to treatment (≥50% reduction of MADRS total score at week four); remission (MADRS total score ≤10 points); a change in Clinical Global Impressions Scale (CGI) scores; and a change in Beck Depression Inventory–Short Form (BDI-SF) scores at the end of the studies.25,26 Dropout rates for any reason were observed so that acceptability of the treatment approaches could be compared.
Statistical Analysis
All analyses were based on the intent-to-treat (ITT) population, which consisted of all randomized patients. The VNF treatment arms from both trials were merged prior to analysis. For comparisons of baseline demographic and clinical variables between treatment groups, one-way analysis of variance, a Kruskal–Wallis test, or a chi-square test was used, as appropriate. The primary efficacy outcome measure (a MADRS score change from baseline to week 4 with the last observation carried forward missing data imputation method) was assessed using an analysis of covariance (ANCOVA; type III sum of squares) with the treatment as a factor, and the baseline MADRS score as a covariate. Additional clinical characteristics (duration of MDD, number of episodes, duration of current episode, and number of adequate treatments in current episodes) were tested for collinearity before they were entered into the analysis. The least-squares means were used to compare treatment groups, multiple comparisons were corrected by Tukey–Kramer’s post hoc test, and Hedges’ g effect size with 95% confidence intervals was calculated. The continuous secondary outcomes (CGI, BDI) were compared in similar analyses of covariance, while visit-wise between-group differences were assessed by repeated-measures analysis of variance (RM ANOVA) with the Greenhouse–Geisser procedure to correct the degrees of freedom, followed by Tukey–Kramer’s pairwise post hoc testing if needed. Categorical secondary outcomes (response, remission, and drop-outs) were analyzed by the chi-square test. All statistical analyses were performed with Stata version 15.1 (StataCorp, Texas, USA).
Results
Patient Characteristics
A total of 117 participants (33 males and 84 females, mean age ± standard deviation (SD) was 45.3 ± 11.7 years) with MDD were included in the analysis (tDCS n=29, rTMS n=29, and VNF n=59). Patient flow and the reasons for discontinuation are presented by treatment group (CONSORT diagram) in Figure 1. Baseline demographic and clinical parameters of the studied population did not differ among groups (Table 1).
 |
Table 1 Baseline Demographic and Clinical Characteristics of Treatment Groups |
Efficacy and Safety Measures
Primary Outcomes
The least squares (LS) mean reduction from baseline to week 4 in the MADRS total scores was 7.67 (95% CI 4.87 to 10.47), 7.02 (4.22 to 9.82), and 8.85 (6.90 to 10.81) for tDCS, rTMS, and VNF (Table 2), respectively, resulting in non-significant differences between treatment groups (ANCOVA; F(2,111)=0.63, p=0.54; LS mean difference: tDCS vs rTMS: 0.65, 95% CI −3.27 to 4.57, p=0.94, Hedges’ g=0.09; tDCS vs VNF: −1.18, −4.57 to 2.21, p=0.77, g=−0.16; rTMS vs VNF: −1.83, −5.22 to 1.56, p=0.54, g=−0.24) (Table 3).
 |
Table 2 Visit-Wise Change in MADRS Scores in the Venlafaxine, rTMS and tDCS Groups |
 |
Table 3 Between-Group Differences in Change of MADRS Score at Week 4 |
Secondary Outcomes
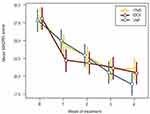
When analyzing the visit-by-visit change in MADRS scores, a nonsignificant between-group difference was revealed (RM ANOVA; visit: F(2.5,279.8)=27.3, p˂0.001; treatment: F(2,112)=0.08, p=0.93; treatment-by-visit interaction: F(5,279.8)=1.80, p=0.11) (Table 2). However, it is worth mentioning that while the MADRS score reduction in the VNF group was gradual across the study period, the majority of improvements in the rTMS and especially in the tDCS groups appeared within the first 2 weeks (Figure 2).
Similarly, neither CGI score changes nor improvements in self-assessment (BDI) indicated difference among groups (ANCOVA; CGI: F(2,111)=2.11, p=0.13; LS mean difference: tDCS vs rTMS: 1.1, 95% CI −0.6 to 2.8, p=0.37; tDCS vs VNF: −0.1, −1.5 to 1.3, p>0.99; rTMS vs VNF: −1.2, −2.6 to 0.3, p=0.15; BDI: F(2,111)=2.33, p=0.10; tDCS vs rTMS: 3.0, 95% CI −1.0 to 7.0; p=0.23; tDCS vs VNF: 0.1, −3.4 to 3.6, p>0.99; rTMS vs VNF: −3.0, −6.5 to 0.5, p=0.14).
Response and remission rates did not differ significantly among treatment groups. In terms of response rates, tDCS reached 24%, rTMS 31%, and VNF 41% (χ2 =2.59, df=2, p=0.28), and remission was found in 17% patients with tDCS, 17% with rTMS, and 27% on VNF (χ2 =1.66, df=2, p=0.44) (Table 4). A total of 20 patients (17%) dropped out of the studies. The proportion of dropouts was not significantly different between treatment groups (tDCS 21%, rTMS 10%, and VNF 19%, χ2 =1.41, df=2, p=0.52).
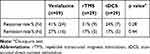 |
Table 4 Response and Remission Rates in Treatment Groups |
There were only three serious adverse events in both studies (rTMS n=1 (hypertension crisis), VNF n=1 (broken leg and hypotension), tDCS n=1 (switch to hypomania)). Adverse events observed in the studies were in line with the previously described side effects for each treatment modality. In addition, the percentages of patients who guessed their treatment in the studies were similar (44–55%).
Discussion
This pooled analysis built on previous findings on the usefulness of rTMS and tDCS, and compared them with VNF, in the treatment of MDD. The results of our study showed comparable efficacy and acceptability across all three. Every analyzed intervention achieved a significant reduction in depressive symptoms by the end of the study. In terms of response, remission, and dropout rates, the intergroup comparison did not reveal any statistical significance.
Generally, there is a lack of head-to-head studies comparing the clinical usefulness of the neurostimulation methods with each other and with ADs. While rTMS seems to be well established in the treatment of MDD,27 the literature on tDCS has shown equivocal results.28,29 Nevertheless, a recent meta-analysis of 23 randomized controlled trials confirmed the efficacy of tDCS, though the effect was considered modest.30 One large multicenter French RCT investigated the efficacy difference of low-frequency rTMS vs VNF in patients with treatment-resistant depression. One-hundred-and-seventy subjects were randomized to active LF rTMS with placebo VNF, active VNF with sham rTMS, and active rTMS with active VNF subgroups. At the endpoint, similar antidepressant effects were reported in all three groups, thus supporting the use of LF rTMS in the treatment of treatment-resistant depression.31 With the exception of our study,21 tDCS has not been compared with VNF in any other RCT. The efficacy and acceptability of tDCS compared with ADs (fluoxetine 20mg, sertraline 50mg, and escitalopram 20mg) were evaluated in three studies.32–34 Mixed results were reported, eg, the older studies found that fluoxetine, sertraline, and tDCS had similar effects. The more recent trial showed the superiority of escitalopram over tDCS. A recently published network meta-analysis indirectly comparing tDCS and LF rTMS did not find significant differences in terms of response and discontinuation rates.29 It is in accordance with our results. The finding that the majority of improvements in both neurostimulation arms (especially in the tDCS group) appeared within the first 2 weeks corresponds well with a recent work that examined different trajectories of response to tDCS in MDD.35 They found that 44% of patients receiving tDCS showed a pattern of rapid improvement, being evident as early as week 1, whereas previous analyses suggested that tDCS would present effects only after the acute treatment phase.
The results of our analysis indicated that all three treatment strategies are safe and well tolerated. Only a few serious adverse effects were reported. We experienced one case of switch to hypomania that may have resulted from the active tDCS treatment. The other cases of adverse effects did not have a clear connection with active treatment. One patient suffered from an episode of hypotension on venlafaxine. One case of hypertension crisis, in a patient previously treated for hypertension, was reported during the first week of active rTMS treatment. Other dropouts were reported due to the patient’s decision or worsening of the symptoms. All approaches confirmed high levels of safety, as was noted earlier. What is worth mentioning in connection with our results is that pharmacotherapy is often associated with side effects such as sexual dysfunction, nausea, weight gain, and insomnia.6 Neurostimulation methods could be considered as an option when there is a need to avoid drug-induced side effects or if the patient has an intolerance to medication. Our findings support the use of tDCS and right LF rTMS stimulation as an effective alternative treatment for MDD patients. Another benefit is the relatively low cost of these neurostimulation treatments; tDCS tends to be less expensive than rTMS. Moreover, patients may be offered the possibility of self-administered home application of tDCS, as this treatment approach has recently shown promising results.36
According to our literature review, no studies have directly compared the efficacy and tolerability of rTMS and tDCS. We analyzed databases from two studies with almost identical protocols. Even though we could not provide a direct comparison, the analogical designs of our studies and the same research center provided more reliable information on the NIBS comparison. However, our results should be treated with caution because the study has several limitations. The main one was the use of a post hoc analysis – the data from the two previous RCTs using VNF and neurostimulation methods (tDCS and rTMS) were pooled. We could therefore only assess the indirect comparison of the neurostimulation methods. (One strength of the study may be that, even though the pooled VNF subgroup comprised almost twice as many patients as the rTMS and tDCS subgroups, the neurostimulation methods were not disadvantaged in terms of the final results.) We compared two neurostimulation treatments, but other protocols are being applied in clinical practice or research trials in MDD treatment. Right LF rTMS is considered an efficacious approach. Level A evidence is also confirmed for left HF rTMS and deep HF-rTMS over the left DLPC. Bilateral rTMS of DLPC is supported with level B evidence. Some novel rTMS protocols for MDD treatment are being investigated, eg, theta-burst stimulation (TBS) with intermittent (level B) and continuous protocols (level C).37 Because there is considerable heterogeneity in rTMS stimulation settings, no clear recommendations for optimal rTMS parameters have been established. The optimal protocol for tDCS treatment has also not been clearly determined; different stimulation parameters, eg duration (20–30 minutes/day), current intensity (1–2 mA), number of treatments (5–20), and cathode placements, have been used in clinical trials.30,38 Most rTMS studies to date primarily recruited patients with high degrees of treatment resistance. It could unfavorably bias the reputation of rTMS.39 On the contrary, tDCS trials were conducted either in non-TRD or included both TRD and non-TRD.30 The proportion of resistant and non-resistant subjects among treatment groups in our study was comparable. So that we could offer the comparison on the effectiveness of rTMS compared to tDCS without mentioned bias of rTMS. The next limitation of our study is, that our analyzed RCTs did not involve a placebo arm in the comparison of antidepressant approaches. As the placebo response in antidepressant trials response range from 35% to 40%40 and regarding recent meta-analysis, also placebo response to rTMS in MDD is large,41 we can assume, that the placebo response may be a component of the therapeutic response to rTMS, tDCS, and VNF in MDD. All subjects in our studies were aware that they will receive an active intervention. It could increase the placebo response.42 It is important to note that all analyzed interventions are considered effective in the MDD treatment. Our ethics committee does not approve a placebo treatment for depressed inpatients from the psychiatry ward. Finally, our analysis evaluates the results from 4-week trials, so we can only comment on the acute treatment of MDD. The 4-week treatment period for effect evaluation in our study was set following the recent aforementioned Canadian guidelines for MDD treatment.43 In clinical practice, the effect of ADs tends to be felt after 4–8 weeks.44 The onset of action of VNF may be delayed in some cases. RTMS treatment in the study was in accord with current recommendations, but a higher number of stimulations are recommended for patients with partial response.37,45 The same applies to tDCS. Therefore, extending the treatment period may be useful to observe the full antidepressant effect.30
Despite these limitations, our findings complement the growing body of evidence for the usefulness of non-invasive neurostimulation methods in clinical practice. There is a need for further clarification on the AD efficacy of different neurostimulation therapies, but our results suggest that patients with MDD could benefit from right low-frequency rTMS, left anodal tDCS, and VNF treatment. A head-to-head, long-term, adequately powered comparison of neurostimulation methods and ADs that identified not only the efficacy of the treatments but also predictors associated with positive outcomes would provide more information about clinical benefits and the possible superiority of one AD approach.
Conclusion
This pooled analysis comprised data from 117 patients who participated in two RCTs comparing rTMS, tDCS, and VNF in the acute treatment of depression. We have found comparable efficacy of all three treatment modalities. The results also indicated that all three treatment strategies are safe and well tolerated, only a few serious adverse effects were reported. In terms of response, remission, and dropout rates, the intergroup comparison did not reveal any statistically significant difference. Based on our results, the patients with MDD may similarly benefit from right low-frequency rTMS, left anodal tDCS, and VNF treatment.
Data Sharing Statement
Data used in our study are available from the corresponding author upon request. The request must comply with confidentiality, Czech and European laws, and ethics rules.
Acknowledgments
This study is supported by the Ministry of Health of the Czech Republic, grant AZV ČR (Czech Health Research Council), number NV18-04-00260. Natalie Görnerova, Jiri Renka, Pavla Stopkova, Miloslav Kopecek, and Libuse Pohlova rated and cared for the study patients.
Disclosure
Dr Tomas Novak reports personal fees from Krka ČR sro, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Murray CJL, Barber RM, Foreman KJ, et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–2191.
2. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–1366. doi:10.1016/S0140-6736(17)32802-7
3. Gibbons RD, Hur K, Brown CH, Davis JM, Mann JJ. Benefits from antidepressants synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):572–579. doi:10.1001/archgenpsychiatry.2011.2044
4. Arroll B, Chin WY, Martis W, et al. Antidepressants for treatment of depression in primary care: a systematic review and meta-analysis. J Prim Health Care. 2016;8(4):325–334. doi:10.1071/HC16008
5. Rush AJ, Trivedi MH, Wisniewski SR, et al. Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med. 2006;354(12):1231–1242. doi:10.1056/NEJMoa052963
6. Kikuchi T, Suzuki T, Uchida H, Watanabe K, Mimura M. Association between antidepressant side effects and functional impairment in patients with major depressive disorders. Psychiat Res. 2013;210(1):127–133. doi:10.1016/j.psychres.2013.05.007
7. McClintock SM, Reti IM, Carpenter LL, et al. Consensus recommendations for the clinical application of repetitive transcranial magnetic stimulation (rTMS) in the treatment of depression. J Clin Psychiatry. 2018;79(1):35. doi:10.4088/JCP.16cs10905
8. Gaynes BN, Lloyd SW, Lux L, et al. Repetitive transcranial magnetic stimulation for treatment-resistant depression: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(5):477–U196. doi:10.4088/JCP.13r08815
9. Berlim MT, van den Eynde F, Tovar-Perdomo S, Daskalakis ZJ. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44(2):225–239. doi:10.1017/S0033291713000512
10. Cao X, Deng CS, Su XL, Guo Y. Response and remission rates following high-frequency vs. low-frequency repetitive transcranial magnetic stimulation (rTMS) over right DLPFC for treating major depressive disorder (MDD): a meta-analysis of randomized, double-blind trials. Front Psychiatry. 2018;9. doi:10.3389/fpsyt.2018.00413
11. Chen JJ, Zhou CJ, Wu B, et al. Left versus right repetitive transcranial magnetic stimulation in treating major depression: a meta-analysis of randomised controlled trials. Psychiat Res. 2013;210(3):1260–1264. doi:10.1016/j.psychres.2013.09.007
12. Berlim MT, Van den Eynde F, Daskalakis ZJ. Clinically meaningful efficacy and acceptability of low-frequency repetitive transcranial magnetic stimulation (rTMS) for treating primary major depression: a meta-analysis of randomized, double-blind and sham-controlled trials. Neuropsychopharmacol. 2013;38(4):543–551. doi:10.1038/npp.2012.237
13. Milev RV, Giacobbe P, Kennedy SH, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. neurostimulation treatments. Can J Psychiatry. 2016;61(9):561–575. doi:10.1177/0706743716660033
14. Berlim MT, Van den Eynde F, Daskalakis ZJ. Clinical utility of transcranial direct current stimulation (tDCS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. J Psychiatr Res. 2013;47(1):1–7. doi:10.1016/j.jpsychires.2012.09.025
15. Shiozawa P, Fregni F, Bensenor IM, et al. Transcranial direct current stimulation for major depression: an updated systematic review and meta-analysis (vol 17, pg 1443, 2014). Int J Neuropsychopharmacol. 2014;17(9):1539. doi:10.1017/S1461145714000807
16. Meron D, Hedger N, Garner M, Baldwin DS. Transcranial direct current stimulation (tDCS) in the treatment of depression: systematic review and meta-analysis of efficacy and tolerability. Neurosci Biobehav Rev. 2015;57:46–62. doi:10.1016/j.neubiorev.2015.07.012
17. Brunoni AR, Moffa AH, Fregni F, et al. Transcranial direct current stimulation for acute major depressive episodes: meta-analysis of individual patient data. Br J Psychiatry. 2016;208(6):522. doi:10.1192/bjp.bp.115.164715
18. Mutz J, Edgcumbe DR, Brunoni AR, Fu CHY. Efficacy and acceptability of non-invasive brain stimulation for the treatment of adult unipolar and bipolar depression: a systematic review and meta-analysis of randomised sham-controlled trials. Neurosci Biobehav Rev. 2018;92:291–303. doi:10.1016/j.neubiorev.2018.05.015
19. Moffa AH, Martin D, Alonzo A, et al. Efficacy and acceptability of transcranial direct current stimulation (tDCS) for major depressive disorder: an individual patient data meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2020;99.
20. Bares M, Kopecek M, Novak T, et al. Low frequency (1-Hz), right prefrontal repetitive transcranial magnetic stimulation (rTMS) compared with venlafaxine ER in the treatment of resistant depression: a double-blind, single-centre, randomized study. J Affect Disord. 2009;118(1–3):94–100. doi:10.1016/j.jad.2009.01.032
21. Bares M, Brunovsky M, Stopkova P, Hejzlar M, Novak T. Transcranial direct-current stimulation (tDCS) versus venlafaxine ER in the treatment of depression: a randomized, double-blind, single-center study with open-label, follow-up. Neuropsychiatr Dis Treat. 2019;15:3003–3014. doi:10.2147/NDT.S226577
22. American Psychiatric Association. Diagnostic Criteria from DSM-IV-TR. American Psychiatric Association; 2000.
23. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The mini-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
24. Montgomery SA, Asberg M. New depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(Apr):382–389. doi:10.1192/bjp.134.4.382
25. Guy W. Clinical global impression. Assessment Man Psychopharmacol. 1976;217–222.
26. Beck AT, Rial WY, Rickels K. Short form of depression inventory – cross-validation. Psychol Rep. 1974;34(3):1184–1186. doi:10.1177/003329417403403s01
27. Baeken C, Brem AK, Arns M, et al. Repetitive transcranial magnetic stimulation treatment for depressive disorders: current knowledge and future directions. Curr Opin Psychiatry. 2019;32(5):409–415. doi:10.1097/YCO.0000000000000533
28. Loo CK, Husain MM, McDonald WM, et al. International randomized-controlled trial of transcranial direct current stimulation in depression. Brain Stimul. 2018;11(1):125–133. doi:10.1016/j.brs.2017.10.011
29. Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu CHY, Young AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. 2019;364.
30. Razza LB, Palumbo P, Moffa AH, et al. A systematic review and meta-analysis on the effects of transcranial direct current stimulation in depressive episodes. Depress Anxiety. 2020;37(7):594–608. doi:10.1002/da.23004
31. Brunelin J, Jalenques I, Trojak B, et al. The efficacy and safety of low frequency repetitive transcranial magnetic stimulation for treatment-resistant depression: the results from a large multicenter French RCT. Brain Stimul. 2014;7(6):855–863. doi:10.1016/j.brs.2014.07.040
32. Rigonatti SP, Boggio PS, Myczkowski ML, et al. Transcranial direct stimulation and fluoxetine for the treatment of depression. Eur Psychiatry. 2008;23(1):74–76. doi:10.1016/j.eurpsy.2007.09.006
33. Brunoni AR, Valiengo L, Baccaro A, et al. The sertraline vs electrical current therapy for treating depression clinical study results from a factorial, randomized, controlled trial. JAMA Psychiat. 2013;70(4):383–391. doi:10.1001/2013.jamapsychiatry.32
34. Brunoni AR, Moffa AH, Sampaio B, et al. Trial of electrical direct-current therapy versus escitalopram for depression. N Engl J Med. 2017;376(26):2523–2533. doi:10.1056/NEJMoa1612999
35. Goerigk SA, Padberg F, Buhner M, et al. Distinct trajectories of response to prefrontal tDCS in major depression: results from a 3-arm randomized controlled trial. Neuropsychopharmacol. 2021;46(4):774–782. doi:10.1038/s41386-020-00935-x
36. Alonzo A, Fong J, Ball N, Martin D, Chand N, Loo C. Pilot trial of home-administered transcranial direct current stimulation for the treatment of depression. J Affect Disord. 2019;252:475–483. doi:10.1016/j.jad.2019.04.041
37. Lefaucheur JP, Aleman A, Baeken C, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018). Clin Neurophysiol. 2020;131(2):474–528.
38. Dedoncker J, Brunoni AR, Baeken C, Vanderhasselt MA. A systematic review and meta-analysis of the effects of transcranial direct current stimulation (tDCS) over the dorsolateral prefrontal cortex in healthy and neuropsychiatric samples: influence of stimulation parameters. Brain Stimul. 2016;9(4):501–517. doi:10.1016/j.brs.2016.04.006
39. Kiebs M, Hurlemann R, Mutz J. Repetitive transcranial magnetic stimulation in non-treatment-resistant depression. Br J Psychiatry. 2019;215(2):445–446. doi:10.1192/bjp.2019.75
40. Furukawa TA, Cipriani A, Atkinson LZ, et al. Placebo response rates in antidepressant trials: a systematic review of published and unpublished double-blind randomised controlled studies. Lancet Psychiatry. 2016;3(11):1059–1066. doi:10.1016/S2215-0366(16)30307-8
41. Razza LB, Moffa AH, Moreno ML, et al. A systematic review and meta-analysis on placebo response to repetitive transcranial magnetic stimulation for depression trials. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:105–113. doi:10.1016/j.pnpbp.2017.10.016
42. Sinyor M, Levitt AJ, Cheung AH, et al. Does inclusion of a placebo arm influence response to active antidepressant treatment in randomized controlled trials? Results from pooled and meta-analyses. J Clin Psychiatry. 2010;71(3):270–279. doi:10.4088/JCP.08r045116blu
43. Kennedy SH, Lam RW, McIntyre RS, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. pharmacological treatments. Can J Psychiatry. 2016;61(9):540–560. doi:10.1177/0706743716659417
44. Henssler J, Kurschus M, Franklin J, Bschor T, Baethge C. Trajectories of acute antidepressant efficacy: how long to wait for response? A systematic review and meta-analysis of long-term, placebo-controlled acute treatment trials. J Clin Psychiatry. 2018;79(3).
45. Perera T, George MS, Grammer G, Janicak PG, Pascual-Leone A, Wirecki TS. The clinical TMS society consensus review and treatment recommendations for TMS therapy for major depressive disorder. Brain Stimul. 2016;9(3):336–346. doi:10.1016/j.brs.2016.03.010