Introduction
The World Health Organization (WHO) declared the outbreak of coronavirus (COVID-19) to be a public health emergency of international concern and the crisis is generating economic and health problem throughout the population.1 Coronavirus disease 2019 (COVID-19) initially broke out in Wuhan, China, in December 2019 and promptly became a worldwide pandemic and global heath threat within few months.2
COVID-19 is the largest outbreak of atypical pneumonia since the severe acute respiratory syndrome (SARS) outbreak in 2003.3 Within a short period of time after the initial outbreak the total number of cases and deaths increased.4
Studies reported that impact of COVID-19 on mental health was higher due to many aspects such as the loss of employment, loss of finances, fear of contamination and death. This increases the prevalence of mental health problems, specially depression and anxiety in quarantined individuals.5
According to the WHO report the pandemic has its own consequences on mental health and psycho-social behavior.1 It reported that that new measures such as self-isolation and quarantine have affected usual activities that may lead to an increase in loneliness, anxiety, depression, drug use, and self-harm or suicidal behavior.1,6 The recent survey done by the Indian Psychiatric Society shows a 20% increase in mental illnesses since the outbreak in India.7
The public health emergencies resulting from COVID-19 are negatively impacting the mental health of the population and increasing the incidence of psychological crises and challenge to psychological resilience.8,9 Recent studies reported that during the COVID-19 outbreak, the depression rate in the general population ranges from 3.7%~48.3%.10–12 In Korea, the first COVID-19 outbreak occurred at a local psychiatric ward. Out of 103 patients held in the psychiatric ward, 102 tested positive for the virus; this shows that mental health problems make it difficult to manage the spread of the virus.13 COVID-19 is more serious and fatal for the elderly and those with underlying health conditions and serious mental illness.14 A study carried out in Colombia reported that there were no differences in anxiety between people who were under full versus and not confirmed quarantined individuals but higher than that of general population.15
Psychologists and mental health professionals reported that the pandemic will impact the mental health of the global population with an increase in cases of depression, suicide, and self-harm, as well as other symptoms reported globally.16–18 Studies carried out in China, Italy, and the USA reported that the prevalence of depression has increased rapidly during the COVID-19 pandemic.19
Mental health and psychosocial consequences of the COVID-19 pandemic may be particularly serious for at least four groups of people: 1) those who have been directly or indirectly in contact with the virus; 2) those who are already ready vulnerable to biological or psychosocial stressors, because of higher level of exposure, and 3) people who are following the news through numerous media channels.20 Studies show that the major adverse consequence of the COVID-19 pandemic are likely to be increased social isolation and loneliness, both of which are strongly associated with anxiety, depression, self-harm, and suicide attempts.21,22 Chronic depression may lead to severe cognitive impairment,23 severe social dysfunction,24 poor quality of life,25,26 and may lead to serious suicidal behavior.27,28 The prevalence of depression in Ethiopia was 6.5% before the pandemic.29
Early identification of the population’s mental health problems allows for the efficient implementation of interventional strategies, according to the findings.
To the best of our knowledge, there have been no previous studies carried out on depression among quarantined individual in Ethiopia.
Methods and Materials
A multi-institution-based cross-sectional study design was conducted from June to October 2020 at Study Tigray emergency and treatment center. Tigrai regional state is in northern Ethiopia, 783 Kilometers north of Addis Ababa, the capital city of Ethiopia. Tigrai regional state has five emergency treatment centers and currently it is also used as quarantine center and three centers was selected randomly using a lottery method. The study was conducted at the selected three treatment centers. The estimated number of quarantined individuals was 3500. All were adult quarantined individuals age ≥ 18 at the selected Tigrai emergency and treatment centers during data collection period.
Sample Size Determination
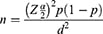
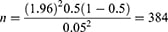
The sample was calculated by using single population formula, using the following assumptions.
Where;
n = sample size
Z = significance level at
= significance level at  0.05
0.05
P = the prevalence of psychological distress among quarantined individual is unknown in our country; hence, P = 50% (0.5) was used.
d = Absolute precision or tolerable margin of error = 0.05
Therefore:
Since the population was less 10.000 a correction formula was used = N*n/n+N+1 = 346
N = Total population = 3500
n = sample size
Considering the sample size was 10% of the none respondent rate, the size yields 346+35 = 381.
Sampling Techniques and Compositions
A simple random sampling technique was used to select study population at Tigrai emergency operation and treatment centers during study period. Sampling frame was obtained from each emergency operation and treatment center and Computer generation was used to select the study participants. Sample was proportionally allocated the three treatment and quarantine centers.
Tools and Data Collection Procedure
Socio-demographic characteristics were collected by structured socio-demographic questionnaires and clinical factors such as duration of quarantine and substance use were also collected by semi-structured questionnaires. Social support was collected by Oslo-3 item social support scale, it is a three item questionnaire, commonly used to assess social support and has been used in several studies. The sum score scale ranges from 3–14, which has three categories: poor support 3–8, moderate support 9–11, and strong support 12–14. Stigma was assessed by the Jacoby three-item Perceived Stigma Scale and those who score 1 and above are considered as having perceived stigma; depression was assessed by depression, anxiety, and stress scale (DASS). Data was collected by face-to-face interviews using the Tigrigna version of the pre-tested questionnaire, adhering to social distancing during the interviews and using personal protective equipment to reduce the transmission of the disease. Training was given to data collectors and supervisors.
Operational Definitions
Depression
A score of 10 and above in DASS-D indicates the presence of depression.30
Social Support
Using OSLo-3 scale categorized in to poor “3–8” moderate “9–11” and strong “12–14.”31
Substance Ever Use
Use of specific substance once in their life time (for non-medical purpose).32
Substance Current Use
Using of specific substance in the last three months (for non-medical purposes).32
Perceived Stigma
Based on the Jacoby Perceived Stigma Scale: a score of 1 and above indicates the patient is stigmatized.33
Data Quality Assurance and Analysis
The data was check, coded, and entered to Epi-data manager version 4.4.1 and was exported to SPSS version 20. The descriptive statistics (frequency, percentage, mean) and charts were done to describe data. Multicollinearity was checked using variance inflation factor (VIF) and tolerance. Binary logistic regression analysis was used. All variables with a p-value of, less than 0.2 at bivariate logistic regression analysis were entered into the multivariable logistic regression model. Multivariable logistic regression analysis was conducted to determine the presence of a statistically significant association between explanatory variables and outcome variables. Hosmer-lemeshow goodness and model fitness was checked and P values less than 0.05 were considered statistically significant and strength of the association was present by odds ratio with 95% C.I.
To control quality of data the questionnaire was translated to Tigrigna and back to English to check consistency. Data collectors were supervised daily and the filled questionnaires were checked daily by the supervisors and principal investigator.
Results
Socio-Demographic Characteristics
In this study initially we hoped to have 381 quarantined participants, but only 371 individuals participated, with a response rate of 97%. AOf the participants 269 (72.5%) were male and 102 (27.5%) were female. The majority of the participants (92.7%) were orthodox Christians. The mean age of the study participants was 27.8, with an SD of 10.4 (See Table 1).
 |
Table 1 Socio-Demographic Characteristics of Quarantined Individuals Due to COVID−19 in Tigrai Quarantine and Treatment Centers Tigrai, Ethiopia, 2020 (n = 371) |
Clinical and Psychosocial Factors of the Study Participants
The mean duration of quarantined individuals was 11.6 with an SD of 1.5. Of the total participants 28.3% (105) had perceived stigma and around 19.4% and 37% of quarantined individuals had poor and moderate social support, respectively (see Table 2).
 |
Table 2 Frequency Distribution of Substance Related Factors of Quarantined Individuals at Tigrai Quarantined and Treatment Centers, Tigrai, Ethiopia, 2020 (n = 371) |
Factors Associated with Depression Among Quarantined Individuals
A binary logistic regression model was used to analyze the data. Bivariate and multivariable logistic regression analysis was carried out and variables with p-value>0.2 in bivariate analysis were exported to multivariable logistic regression analysis to see a further association. In bivariate logistic regression analysis sex, marital status, job, social support, and perceived stigma were with a p-value of >0.2 and exported to multivariable logistic regression analysis. Multivariable logistic regression analysis was performed and factors such as being female, duration of quarantine, unemployment, and having perceived stigma were significantly associated with depression with a p-value less than 0.05.
The odds of depression among quarantined individuals due to COVID-19 was about 2.5 (AOR 2.5, 95% CI [1.2–5.4]) times higher among female quarantined individuals than male quarantined individuals. As the duration of quarantine increased by one unit depression among quarantined individuals increased by 1.3. Quarantined Individuals with perceived stigma were about 12 (AOR, 12.9, 95% CI [6.0–27.9]) times more likely to have depression than those who had no perceived stigma. In this study, 54% (AOR 0.46, 95% CI, [0.22–0.96]) of unemployed quarantined individuals were less likely to develop depression than those employed individuals (Table 3).
Discussion
The prevalence of depression among quarantined individuals was 18.1% with 95% CI (13.7–22).
In this study, depression among quarantined individuals was lower than studies conducted in affected areas of China, which was 35.9% and 26.5% in two different studies.34,35 This discrepancy might be due to higher numbers of cases in China during the study period and low numbers of cases and deaths.
A study carried out in southwestern China in early February 2020 was lower than this study.36 Another study carried out in Italy showed that the prevalence of depression was lower than this current study. This difference might be the study period time and that the study carried out in Italy was on population, whereas this study was on quarantined individuals.37
In this study factors associated with depression among quarantined individuals were: being female, duration of quarantine, unemployment, and perceived stigma. This was supported by studies carried out in China, Italy, Spain, and Japan.36,38–41 In the current study, as the duration of quarantine increased by one unit, depression among quarantined individuals increases by 1.3. This might be due to individuals being unable to adapt to a new environment and prolonged periods of loneliness.
The odd of depression among quarantined individuals due to COVID-19 was about 2.5 times higher among female quarantined individuals than male quarantined individuals. This might be because females are less likely to express their feelings than men due to sociocultural influences. Quarantined Individuals with perceived stigma were about 12 times more likely to have depression than those who had no perceived stigma. The possible explanation for this finding might be that COVID-19 is a highly contagious disease and is easily spread across the world.1 So quarantined individuals might perceive fear of stigma and avoidance which may lead them to depression.
Conclusion and Recommendation
The prevalence of depression among quarantined individuals during the COVID 19 pandemic was higher than the general population. In multivariable logistic regression analysis being female, duration of quarantine, unemployment, and having perceived stigma were significantly associated with depression. So clinicians, mental health professionals, and policymakers should work together to address the problem.
Limitations of the Study
The study design was cross-sectional which does not provide a cause-and-effect relationship between variables. Whether participants may or may not have been previously diagnosed with depression is not known.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization.
Data Sharing Statement
The data sets used and analyzed during this study are available from the corresponding author if needed.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the ethical review committee Adigrat University and formal letter of permission was obtained from Adigrat University. This research was conducted by the declaration of Helsinki. The data collectors clearly explained the aims of the study for study participants. The right was given to the study participants to refuse or discontinue participation at any time they want and the chance to ask anything about the study and data collection was started right after obtained consent from participants. All personnel information was kept entirely anonymous and confidential.
Acknowledgments
First and foremost, we would like thank Adigrat University for its financial support. Our recognition also goes to data collectors and supervisors. Finally, we would like to thank the study participants who were willing to take part in this study.
Author Contributions
All authors made a significant contribution to the work reported: whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Adigrat University provided funding: the funder has no role in the design, analysis, preparation of the manuscript and decision to publish.
Disclosure
All authors declared that they have no conflicts of interest for this work.
References
1. World Health Organization. Mental Health and Psychosocial Considerations During the COVID-19 Outbreak, 18 March 2020. World Health Organization; 2020.
2. Rubinow D. Brain, behavior, and immunity: an interactive system. J Natl Cancer Inst Monogr. 1990;(10):79–82.
3. Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49(1):1–3.
4. Kucharski AJ, Russell TW, Diamond C, et al. Early dynamics of transmission and control of COVID-19: a Mathematical Modelling Study. Lancet Infect Dis. 2020;20(5):553–558. doi:10.1016/S1473-3099(20)30144-4
5. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
6. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi:10.1056/NEJMp2008017
7. Loiwal M. 20% Increase in patients with mental illness since coronavirus outbreak: survey. India Today. 2020.
8. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a Retrospective Cohort Study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
9. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi:10.1016/S0140-6736(20)30185-9
10. Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. 2020;51:102092. doi:10.1016/j.ajp.2020.102092
11. Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924. doi:10.1371/journal.pone.0231924
12. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
13. Kim S-W, Su K-P. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. 2020;87:4–5. doi:10.1016/j.bbi.2020.03.025
14. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. doi:10.1016/S2468-2667(20)30061-X
15. Rosen Z, Weinberger-Litman SL, Rosenzweig C, et al. Anxiety and distress among the first community quarantined in the US due to COVID-19: psychological implications for the unfolding crisis. 2020.
16. Li W, Yang Y, Liu Z-H, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732. doi:10.7150/ijbs.45120
17. Moukaddam N, Shah A. Psychiatrists beware! The impact of COVID-19 and pandemics on mental health. Psychiatr Times. 2020;37(3):11–12.
18. Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi:10.1016/S2215-0366(20)30090-0
19. Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2020;30(1):1–2. doi:10.1080/09638237.2020.1757052
20. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):1–4. doi:10.1192/j.eurpsy.2019.3
21. Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Public Health. 2020;17(6):2032. doi:10.3390/ijerph17062032
22. Elovainio M, Hakulinen C, Pulkki-Råback L, et al. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank Cohort Study. Lancet Public Health. 2017;2(6):e260–e266. doi:10.1016/S2468-2667(17)30075-0
23. Semkovska M, Quinlivan L, O’Grady T, et al. Cognitive function following a major depressive episode: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6(10):851–861. doi:10.1016/S2215-0366(19)30291-3
24. Tunvirachaisakul C, Gould RL, Coulson MC, et al. Predictors of treatment outcome in depression in later life: a systematic review and meta-analysis. J Affect Disord. 2018;227:164–182. doi:10.1016/j.jad.2017.10.008
25. Sharma A, Pillai DR, Lu M, et al. Impact of isolation precautions on quality of life: a meta-analysis. J Hosp Infect. 2020;105(1):35–42. doi:10.1016/j.jhin.2020.02.004
26. Ebert DD, Buntrock C, Reins JA, Zimmermann J, Cuijpers P. Efficacy and moderators of psychological interventions in treating subclinical symptoms of depression and preventing major depressive disorder onsets: protocol for an individual patient data meta-analysis of randomised controlled trials. BMJ Open. 2018;8(3):e018582. doi:10.1136/bmjopen-2017-018582
27. Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018;212(5):279–286. doi:10.1192/bjp.2018.27
28. Ernst M, Kallenbach-Kaminski L, Kaufhold J, et al. Suicide attempts in chronically depressed individuals: what are the risk factors? Psychiatry Res. 2020;287:112481. doi:10.1016/j.psychres.2019.112481
29. Bitew T. Prevalence and risk factors of depression in Ethiopia: a review. Ethiop J Health Sci. 2014;24(2):161–169. doi:10.4314/ejhs.v24i2.9
30. Tran TD, Tran T, Fisher J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry. 2013;13(1):24. doi:10.1186/1471-244X-13-24
31. Dalgard OS, Dowrick C, Lehtinen V, et al. Negative life events, social support and gender difference in depression. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–451. doi:10.1007/s00127-006-0051-5
32. Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro MG; World Health Organization. The alcohol, smoking and substance involvement screening test (ASSIST): manual for use in primary care. 2010.
33. Jacoby A. Felt versus enacted stigma: a concept revisited: evidence from a study of people with epilepsy in remission. Soc Sci Med. 1994;38(2):269–274. doi:10.1016/0277-9536(94)90396-4
34. Nie X-D, Wang Q, Wang M-N, et al. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int J Psychiatry Clin Pract;2020;1–6. doi:10.1080/13651501.2020.1791345
35. Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. 2020;1–15.
36. Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med Sci Monit. 2020;26:e924609–924601. doi:10.12659/MSM.924609
37. Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17(9):3165. doi:10.3390/ijerph17093165
38. Peng M, Mo B, Liu Y, et al. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J Affect Disord. 2020;275:119–124. doi:10.1016/j.jad.2020.06.035
39. Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17(13):4779. doi:10.3390/ijerph17134779
40. Pérez-Fuentes M, Molero Jurado M, Martos Martínez Á, Gázquez Linares JJ. Threat of COVID-19 and emotional state during quarantine: positive and negative affect as mediators in a cross-sectional study of the Spanish population. PLoS One. 2020;15(6):e0235305. doi:10.1371/journal.pone.0235305
41. Hirano Y, Aramaki K, Ota S. Factors associated with the mental health of adolescent university students during COVID-19 quarantine in Japan. 2020.