March 10, 2021
2 min read
Source/Disclosures
Dwyer reports receiving research support from the AACAP Junior Investigator Award, the Klingenstein Third Generation Foundation and the NIMH, as well as having served as a consultant for Axsome Therapeutics. Please see the study for all other authors’ relevant financial disclosures.
Intravenous ketamine appeared well-tolerated acutely and had significant short-term efficacy in depressive symptom reduction among adolescents with depression, according to study results published in American Journal of Psychiatry.
“Case reports suggested early potential efficacy of intravenous ketamine in adolescent treatment-resistant depression and intranasal ketamine in bipolar depression,” Jennifer B. Dwyer, MD, PhD, of the Yale Child Study Center at Yale School of Medicine, and colleagues wrote. “Recently a small open-label trial of intravenous ketamine in 13 adolescents with treatment-resistant depression also suggested that ketamine might be effective in this population, although the lack of placebo in the study complicates interpretation of the results. Placebo response rates are high in depression trials, and are particularly high in pediatric depression trials, and it is critical to discriminate genuine drug effects from nonspecific effects.”
Reference: Dwyer JB, et al. Am J Psychiatry. 2021;doi:10.1176/appi.ajp.2020.20010018.
The investigators conducted the current randomized placebo-controlled clinical trial to assess the safety and efficacy of intravenous ketamine in pediatric populations. They administered a single intravenous infusion of either 0.5 mg of ketamine or 0.045 mg of midazolam, and the alternate compound 2 weeks later, to 17 adolescents aged 13 to 17 years with a diagnosis of major depressive disorder. Participants had previously tried one or more antidepressant medication and met the severity criterion of a score of 0.4 on the Children’s Depression Rating Scale-Revised. Score on the Montgomery-Åsberg Depression Rating Scale (MADRS) 24 hours after treatment served as the primary outcome measure.
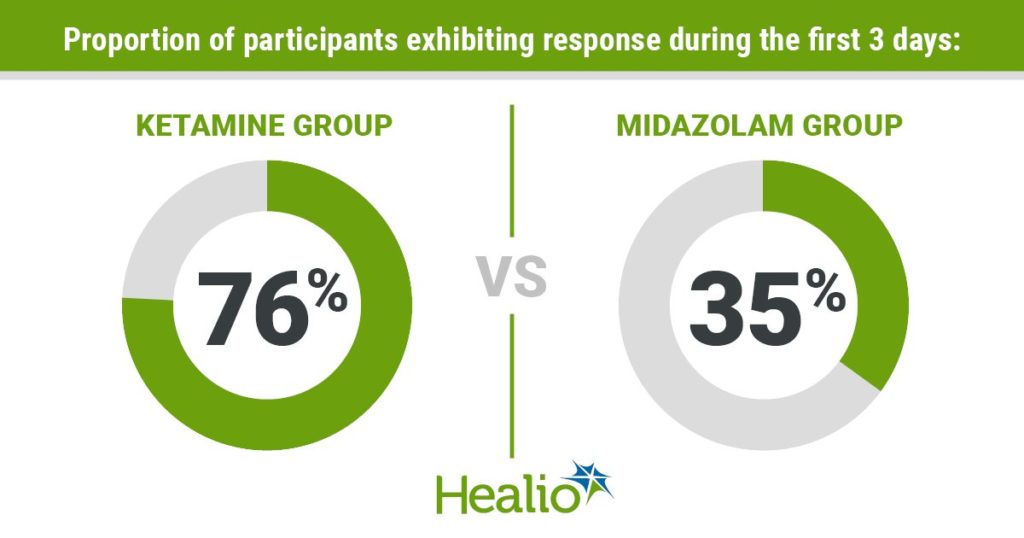
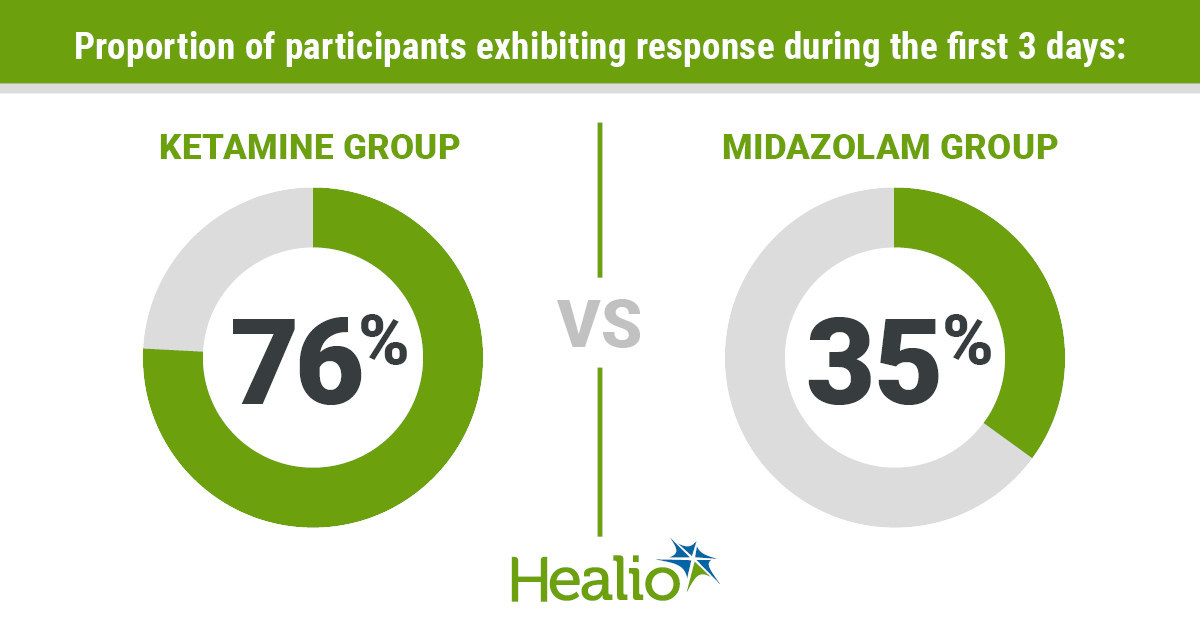
Results showed a significant reduction in depressive symptoms 24 hours after a single ketamine infusion vs. midazolam. Secondary analyses revealed treatment gains linked to ketamine appeared to remain 14 days after treatment, which was the latest time point assessed, according to MADRS but not as measured by the Children’s Depression Rating Scale-Revised. During the first 3 days after infusion, a significantly greater proportion of participants exhibited a response to ketamine vs. midazolam, at 76% and 35%, respectively. The researchers reported no serious adverse events; however, ketamine was linked to transient, self-limited dissociative symptoms that affected participant blinding.
“Further studies are needed to replicate these findings and to better characterize the durability of ketamine’s antidepressant responses in the intermediate and longer term,” Dwyer and colleagues wrote. “Future studies must also pay close attention to neurodevelopmental context and to appropriate safety monitoring in this vulnerable population. Additional data on the safety and efficacy of ketamine are needed before any recommendations regarding integration into care in the non-research population can be made.”