BACKGROUND
Depression and anxiety disorders are together responsible for 8% of years lived with disability globally. Contrary to widely held preconceptions, these are not diseases of affluence. Within a given location, those with the lowest incomes are typically 1.5 to 3 times more likely than the rich to experience depression or anxiety.
ADVANCES
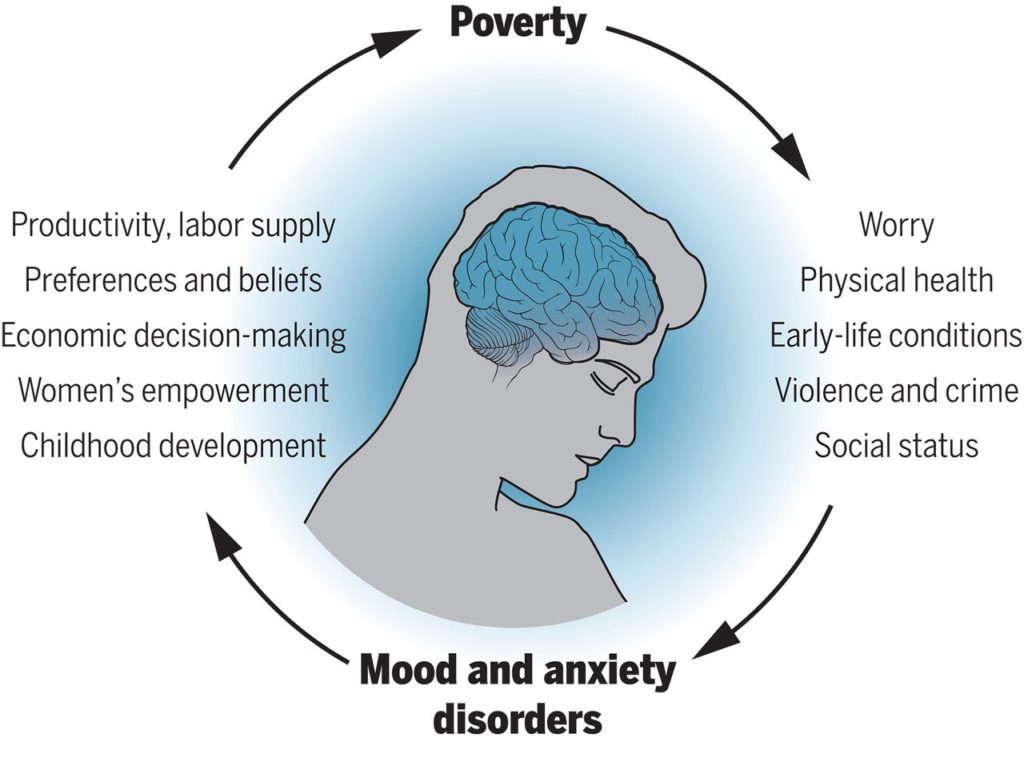
Recent research has established a bidirectional causal relationship between poverty and mental illness. Researchers have begun to isolate the underlying mechanisms, which can guide effective policies to protect the mental health of those living in poverty.
We now know that loss of income causes mental illness. Negative income shocks, such as bad harvests due to poor rainfall or job losses due to factory closures, worsen mental health. Conversely, cash transfers and broader antipoverty programs reduce depression and anxiety in randomized trials. Multiple mechanisms mediate this causal chain. Poverty is associated with volatile income and expenditures. The resulting worries and uncertainty can worsen mental health. Providing health, employment, or weather insurance, or other ways of smoothing shocks, may thus lower depression and anxiety. Living in inadequate housing in low-income neighborhoods, the poor are also more exposed to environmental stresses such as pollution, temperature extremes, and challenging sleep environments, which can cause mental illness. Early-life conditions—poverty experienced in childhood and in utero—increase the likelihood of poor nutrition and other stressors, resulting in impaired cognitive development and adult mental illness. This makes a strong case for providing financial support to pregnant women and caregivers of young children. Poverty is also associated with worse physical health; greater exposure to trauma, violence, and crime; and lower social status, each of which may affect mental health.
Mental illness in turn worsens economic outcomes for individuals. Studies show that randomized interventions to treat mental illnesses increase days worked. Depression and anxiety directly affect the way people think, by capturing their attention and distorting their memory. Such effects are likely to influence economic preferences and beliefs and thus distort important economic decisions made by individuals, such as how much to work, invest, and consume. Reduced concentration and greater fatigue reduce work productivity, and the social stigma of mental illness may further worsen labor-market outcomes. Mental illness appears to increase the likelihood of catastrophic health expenditures for individuals through its comorbidity with chronic illnesses such as diabetes and heart disease. Mental illness may also hinder education and skill acquisition among youth and exacerbate gender inequalities through its disproportionate prevalence among women. Parental mental illness can also influence children’s cognitive development and educational attainment, transmitting mental illness and poverty across generations.
OUTLOOK
The burden of mental illness is likely to increase in the coming decades. Although richer individuals within a given location are less likely to be mentally ill, richer countries do not have lower rates of mental illness. Thus, aggregate economic growth alone is unlikely to reduce mental illness. Climate change is likely to worsen mental health, both directly through the effect of higher temperatures on mood and through reductions in agricultural yields because of changes in rainfall and water supply, more frequent weather-related disasters, and an increased likelihood of violent conflict. Technological change and globalization create large overall economic gains but also concentrated groups of losers whose mental health may be compromised. The spread of social media and associated technologies may also be harming mental health, especially among adolescents.
Policy action on mental health is vital, as is interdisciplinary research on the mechanisms that link poverty and mental illness. Recently developed approaches to psychotherapy, delivered through nonspecialist providers, provide a scalable and effective approach to improving mental health in low-income countries. Given the associated economic benefits of improved mental health, such interventions should be a part of the antipoverty toolkit alongside more traditional economic interventions. Understanding the most effective combination of economic and psychological support in different populations is an important next step. A priority for research is testing for a mental health–based “poverty trap.”If such poverty traps exist, then powerful one-time interventions will have large long-run effects as gains in mental health and economic outcomes reinforce one another. Evaluations of economic interventions should routinely measure mental health, and long-run evaluations of mental health interventions should measure potential impacts on poverty and other key economic outcomes. The causal relationship between poverty and mental health is even more pertinent given the ongoing pandemic, which has disproportionately affected the poor and may have lasting impacts on their economic and mental well-being. A massive investment in mental health was already long overdue. It has now become critically urgent.
This schematic shows the principal mechanisms we identify, on the basis of theory and empirical evidence, through which poverty and depressive and anxiety disorders interact.