Ayse Irem Sonmez,1,2 Charles P Lewis,1 Arjun P Athreya,3 Julia Shekunov,2 Paul E Croarkin2
1Department of Psychiatry and Behavioral Sciences, University of Minnesota Medical School, Minneapolis, MN, USA; 2Department of Psychiatry and Psychology, Mayo Clinic, Rochester, MN, USA; 3Department of Molecular Pharmacology &Experimental Therapeutics, Mayo Clinic, Rochester, MN, USA
Correspondence: Ayse Irem Sonmez
Department of Psychiatry and Behavioral Sciences, University of Minnesota Medical School, 2312 S 6th St, Minneapolis, MN, 55454, USA
Tel +1 612-273-8383
Email [email protected]
Introduction: Major depressive disorder (MDD) is a common condition with heterogeneous presentations that often include predominant anhedonia. Previous studies have revealed that childhood trauma is a potent risk factor for the development of MDD; however, the clinical implications of this finding are not fully understood.
Methods: Participants were adolescents (age 13– 21 years) with a diagnosis of moderate-to-severe major depressive disorder and healthy controls. We used generalized linear models to assess the relationship between anhedonia severity and trauma severity in a cross-sectional dataset.
Results: This cross-sectional analysis of an adolescent sample that underwent clinical evaluations and a trauma assessment, suggested that anhedonia was associated with historical trauma severity. The association between anhedonia and sexual abuse was greater in female participants compared to male participants.
Discussion: Our results were partially in line with the reported literature in adult samples. Future studies aiming to characterize the trauma–anhedonia relationship in adolescents should utilize scales designed specifically to measure these constructs in young populations, and scales that assess specific subtypes of anhedonia.
Introduction
Anhedonia is defined as impaired interest and inability to experience pleasure in previously enjoyable activities.1 Anhedonia is a long accepted core feature of major depressive disorder (MDD) that varies independently of other depressive symptomatology.2 Anhedonia is also recognized as an important component of schizophrenia and post-traumatic stress disorder (PTSD),3 as well as a contributor to suicide risk.4 Increasingly, anhedonia is conceptualized as a transdiagnostic dimension5 with multiple risk pathways leading to its emergence.6
Previous studies have revealed that childhood trauma is a potent risk factor for the development of MDD; however, the impact of childhood trauma on specific depressive symptoms, is inadequately understood. MDD co-occurs in approximately half of individuals with PTSD7 and is common in other trauma-exposed individuals.8 Studies of patients with PTSD suggest that anhedonia may link traumatic experiences anddevelopment of depressive disorders.9
In previous studies with young adult participants, perceived stress has been found to increase negative affect and anhedonia.10 In another study with adults anhedonia was suggested to be the optimal target phenotype when examining the impact of childhood adversity on depression.11 The aim of this study was to investigate the association between anhedonia and past trauma in adolescents. We examined the trauma–anhedonia relationship in healthy adolescents, depressed adolescents, and the combined sample. We hypothesized that anhedonia would demonstrate positive correlations with the severity of various types of childhood traumas.
Methods
Overview
This study was a retrospective, secondary analysis of cross-sectional data from a study conducted by our research group that examined excitatory/inhibitory cortical physiology and glutamatergic neurochemistry in diverse groups of depressed adolescents and healthy youth. Written informed consent was obtained from parents or guardians of participants under 18 years of age, and directly from participants ≥ 18 years.12 Written assents were obtained from participants < 18 years. All research procedures were approved by the Mayo Clinic institutional review board (Rochester, MN, USA). This study was conducted in accordance with the Declaration of Helsinki.
Participants and Eligibility
Depressed participants were adolescents (age 13–21 years) with a diagnosis of a moderate-to-severe major depressive disorder for whom treatment with an antidepressant medication (SSRI) was indicated (but not administered). Healthy control adolescents (age 13–21 years) had no history of psychiatric disorder or treatment. The total number of participants was 56. The parent study was a cross-sectional biomarker study of MDD. No treatment was provided or administered in the form of antidepressant SSRI medications, repetitive transcranial magnetic stimulation (rTMS), or psychotherapy. Contraindications to MRI/MRS, as determined by the MRI safety screen and MRI safety codes were among exclusion criteria. Adolescents in the healthy control group had no current or historical psychiatric diagnosis and no current or previous psychopharmacologic or psychotherapeutic treatment. Participants in the depressed group had current diagnoses of unipolar depressive disorders on the K-SADS-PL diagnostic interview. Exclusion criteria consisted of lifetime history of mania or psychosis, the presence of an active substance use disorder (except nicotine), and any unstable medical condition.
Assessments
Participants were interviewed by a board-certified child and adolescent psychiatrist (PEC) using the Schedule for Affective Disorders and Schizophrenia for School Aged Children, K-SADS-PL.13 Depressive symptom severity was rated with the Children’s Depression Rating Scale, Revised (CDRS-R).14 A score that combined CDRS-R items 2 and 3 (“Difficulty having fun” and “Social Withdrawal”) was used to measure anhedonia (“CDRS-R Anhedonia Subscale”). Participants also completed the Quick Inventory of Depressive Symptomatology (17-item) Adolescent and Parent Self Report (QIDS-A17-SR).15 Prior psychometric studies have demonstrated that CDRS-R and QIDS-A17-SR are reliable and valid instruments for assessing adolescents.15,16 A study from our group, suggested that QIDS-A17-SR has more clinical utility compared to CDRS-R when assessing depression severity.17 In a more recent review, the validity of CDRS-R as measurement of depression symptom severity in adolescents remained unclear.18 As a result of these related findings, depression symptoms severity was assessed with QIDS-A17-SR in the present study.
Participants’ self-reported trauma histories were assessed with the Childhood Trauma Questionnaire (CTQ),19 which is comprised of 28 items, each rated on a five-point Likert scale. In addition to a total trauma score, five subscales are generated: emotional abuse (EAS), physical abuse (PAS), sexual abuse (SAS), physical neglect (PNS), and emotional neglect (ENS). Higher scores on the CTQ denote greater historical trauma severity. The CTQ was used as a continuous variable of trauma severity (total and subscale scores) to increase power and to evaluate trauma as a dimensional variable. CTQ has been used as a continuous variable in the literature recently.20,21
Statistical Analysis
All analyses were conducted using SPSS version 25 (IBM Corp., Armonk, NY, USA). We assessed assumptions of normality with the Shapiro–Wilk test. Non-parametric tests were used to compare data that did not have a normal distribution. Demographics and clinical measures were compared between groups using Student’s t-test, Mann–Whitney U or Chi square. Sex differences across groups were assessed with Chi-Square. Age and QIDS-A17-SR compared with two samples t-test. CDRS-R total score, Anhedonia subscale score and all CTQ scores were compared with Mann–Whitney U as these variables did not have a normal distribution.
Participants were categorized based on prior trauma with scoring cut-off from the CTQ scoring guidelines.19 The “No Trauma” group included participants who scored equal or less than 8 in emotional abuse score, equal or less than 7 in physical abuse score, equal or less than 5 in sexual abuse score, equal or less than 9 emotional neglect score, equal or less than 7 in physical neglect score (Table 1). All other participants were categorized into the “Trauma Exposure “group which indicated that participants had low, moderate or high trauma in at least one subscale.
 |
Table 1 Childhood Trauma Questionnaire Cutoff Scores |
We used generalized linear models to assess the relationship between anhedonia severity and trauma severity. The dependent variables were CTQ scores (total and subscales). The CDRS-R Anhedonia Subscale was the independent variable. Model was built 1) without any covariates 2) controlling for QIDS-A17-SR (proxy for depression severity), age and sex. Akaike’s Information Criterion (AIC) was utilized to assess goodness of fit.
Results
Sample Characteristics
Data from 42 participants (17 healthy controls, 25 depressed; 59.5% female, age range 13–21) were analyzed. Demographics are summarized in Table 2 There were no differences in age or sex between healthy and depressed groups. CTQ scores ranged between 25 and 66. Depressed participants demonstrated significantly higher trauma.
 |
Table 2 Demographics and Clinical Features |
Twenty-four participants reported some level of trauma in any of the five subscales of CTQ based on cut-off scores according to CTQ Manual (Table 1). Age and sex did not differ across two trauma levels. Anhedonia score was significantly higher in the Trauma Exposure group. Full list of medications, comorbidities and reported trauma levels in CTQ subscales were summarized in Table 3. Most frequent comorbidities were ADHD (n=6) and cannabis use disorder (n=7). One participant met criteria for PTSD.
 |
Table 3 Sample Characteristics |
Assessment of Trauma Severity and Anhedonia
There were significant positive relationships between the CDRS-R Anhedonia Subscale and CTQ total score, EAS, ENS, PAS and PNS (all p<0.05), but not SAS, in the combined sample (Table 4). Among the subscales, the EAS showed the most robust association (highest coefficient) (β=0.93, p<0.001). Age did not have a significant relationship with the dependent variable therefore age was not controlled for in any of the models.
 |
Table 4 Generalized Linear Model Results |
The correlation between CDRS-R Anhedonia Subscale and QIDS-A17-SR was r=0.801 (p< 0.001). When QIDS-A17-SR score was added to the models to control for depression severity, the parameter estimates for anhedonia were non-significant in all models.
The main effect of diagnosis was factored in the models as a group along with the interaction of group by anhedonia score. Interaction terms were not significant in any of the models. Similarly, main effect of sex and interaction term sex by anhedonia scores were factored into the models. The interaction term was significant in the sexual abuse scale (Table 5). Figure 1 summarizes the graph of predicted values of sexual abuse scale by anhedonia scores.
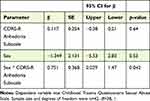 |
Table 5 Association of Sexual Abuse Score with Sex and Anhedonia Score |
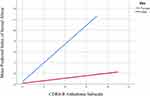 |
Figure 1 CTQ Sexual Abuse Scale by Anhedonia in Males and Females. |
Discussion
The present study sought to examine the association between anhedonia and past trauma in a sample of healthy and depressed adolescents. In the combined sample, anhedonia was associated broadly with trauma measures (total CTQ score and all subscales, except SAS), although these relationships were nonsignificant when corrected for depression severity. This is likely due to covariance between anhedonia and depression severity. In the present study, the correlation between these variables were significant. Also trauma and depression are often collinear parameters, as demonstrated in population-level studies22 adding to the covariance of parameters.
In one prior study Fan and colleagues assessed a young adult sample (18–35 years) using the CTQ and three separate anhedonia-specific scales23 and found that MDD patients with moderate-to-severe childhood trauma had elevated state anhedonia compared to MDD patients with no/low trauma. State anhedonia was measured by Beck Inventory of Depression. We believe this is in line with our findings showing significant positive relationship of anhedonia and trauma. Fan and colleagues also reported that between depressed participants with trauma exposure had greater emotional abuse/neglect scales compared to healthy controls with trauma exposure. This was also noted in our sample despite small sample sizes of 4 healthy controls and 20 depressed participants who reported trauma. In our present study, the main effect of childhood trauma on anhedonia was not qualified further by a significant interaction of diagnosis. This was most likely due to the small sample sizes in our study.
A longitudinal study examining effects of maltreatment found that emotional abuse/neglect predicted depressed mood and anhedonia, with emotional neglect also predicting increased anhedonia over time.24 This raises questions about the cumulative effects of trauma and differential impacts of maltreatment at different stages of social development. This also suggests that childhood adversity imparts later-onset anhedonia in adulthood.
In a prior study that investigated specific types of childhood adversity and social and cognitive capacity, verbal abuse and fear of abuse were found to be significantly associated with worse social motivation. Our findings are partially in line with this study. Physical neglect in our sample unlike the mentioned study results, had smaller parameter estimates compared to emotional abuse however both types of trauma were associated with state anhedonia which we believe covers the domain of social motivation.25
Sexual abuse has been associated with various psychopathology.26,27 Our study was the first in the literature to report a differential effect of sex on the association between sexual abuse and anhedonia in adolescents. In this sample, the association between sexual abuse and anhedonia was stronger in female participants compared to male participants. These results could serve as a foundation for generating new hypothesis on this area.
Some other limitations apply to our findings. The CTQ is completed retrospectively, and the scores could be influenced by the inherent subjectivity and/or current mood state of the participants. Cross-sectional analyses also cannot causally link prior trauma and current depressive symptoms. Assessing anhedonia with two items from a depression scale may not be descriptive enough to appropriately measure all aspects of anhedonia and likely to is influenced by the participant’s mood state at the time of assessment.
Future studies aiming to characterize the trauma–anhedonia relationship in adolescents should utilize scales designed specifically to measure these constructs in young populations, and scales that assess specific subtypes of anhedonia. Similarly, newer conceptualizations of childhood adversity, such as fragmented or chaotic early environmental stimuli, are currently under study as contributors to development of anhedonia via effects on developing reward circuits.28 Novel instruments measuring early life unpredictability have correlated with anhedonia in various cohorts, including adolescents,29 and may enhance our understanding of adversity-related antecedents to development of anhedonia in future clinical studies.
Longitudinal observational studies in larger cohorts are also necessary to eliminate recall bias and establish temporal relationships when measuring outcomes of childhood trauma. If replicated, measures of anhedonia could be considered for future efforts focused on trauma screening.
Funding
This publication was made possible by CTSA Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH) and National Institute of Mental Health Grants R01 MH124655 and R01 MH113700. This work was supported by grants from the Brain & Behavior Research Foundation (C.P.L., 2018 NARSAD Young Investigator Grant 27488, Alan G. Ross Memorial Investigator). The content of this manuscript is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the National Institutes of Mental Health.
Disclosure
Dr. Croarkin has received research grant support from Pfizer, Inc; equipment support from Neuronetics, Inc; equipment support from MagVenture, Inc; and supplies and genotyping services from Assurex Health, Inc for investigator-initiated studies. He was the primary investigator for a multicenter study funded by Neuronetics, Inc and a site primary investigator for a study funded by NeoSync, Inc. Dr. Croarkin has served as a consultant for Procter & Gamble Company, Myriad Neuroscience, Sunovion, and Engrail Therapeutics, Inc. Dr. Lewis reports grants from Brain and Behavior Research Foundation, during the conduct of the study; and site investigator for multicenter trials sponsored by Neuronetics, Inc. and NeoSync, Inc. The authors report no other conflicts of interest in this work.
References
1. Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev. 2011;35(3):537–555.
2. Drysdale AT, Grosenick L, Downar J, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med. 2017;23(1):28–38. doi:10.1038/nm.4246
3. Shankman SA, Katz AC, DeLizza AA, Sarapas C, Gorka SM, Campbell ML. The different facets of anhedonia and their associations with different psychopathologies. In: Anhedonia: A Comprehensive Handbook Volume I. Springer; 2014:3–22.
4. Ducasse D, Dubois J, Jaussent I, et al. Association between anhedonia and suicidal events in patients with mood disorders: a 3‐year prospective study. Depress Anxiety. 2020;38(1):17–27. doi:10.1002/da.23072
5. Husain M, Roiser JP. Neuroscience of apathy and anhedonia: a transdiagnostic approach. Nat Rev Neurosci. 2018;19(8):470–484. doi:10.1038/s41583-018-0029-9
6. Cohen JR, McNeil S, Menon SV. Childhood Maltreatment and Anhedonic Symptoms: test of a Dual-risk Model in Emerging Adults. J Interpers Violence. 2020;886260520969242. doi:10.1177/0886260520969242
7. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi:10.1001/archpsyc.1995.03950240066012
8. Teicher MH, Samson JA. Childhood maltreatment and psychopathology: a case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am j Psychiatry. 2013;170(10):1114–1133. doi:10.1176/appi.ajp.2013.12070957
9. Franklin CL, Zimmerman M. Posttraumatic stress disorder and major depressive disorder: investigating the role of overlapping symptoms in diagnostic comorbidity. J Nerv Ment Dis. 2001;189(8):548–551. doi:10.1097/00005053-200108000-00008
10. Pizzagalli DA, Bogdan R, Ratner KG, Jahn AL. Increased perceived stress is associated with blunted hedonic capacity: potential implications for depression research. Behav Res Ther. 2007;45(11):2742–2753. doi:10.1016/j.brat.2007.07.013
11. Agrawal A, Nelson EC, Littlefield AK, et al. Cannabinoid receptor genotype moderation of the effects of childhood physical abuse on anhedonia and depression. Arch Gen Psychiatry. 2012;69(7):732–740. doi:10.1001/archgenpsychiatry.2011.2273
12. Sonmez AI, Lewis CP, Port JD, et al. Glutamatergic Correlates of Bipolar Symptoms in Adolescents. J Child Adolesc Psychopharmacol. 2020;30(10):599–605. doi:10.1089/cap.2020.0082
13. Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi:10.1097/00004583-199707000-00021
14. Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary studies of the reliability and validity of the Children’s Depression Rating Scale. J Am Acad Child Psychiatry. 1984;23(2):191–197. doi:10.1097/00004583-198403000-00011
15. Bernstein IH, Rush AJ, Trivedi MH, et al. Psychometric properties of the Quick Inventory of Depressive Symptomatology in adolescents. Int J Methods Psychiatr Res. 2010;19(4):185–194. doi:10.1002/mpr.321
16. Mayes TL, Bernstein IH, Haley CL, Kennard BD, Emslie GJ. Psychometric properties of the Children’s Depression Rating Scale-Revised in adolescents. J Child Adolesc Psychopharmacol. 2010;20(6):513–516. doi:10.1089/cap.2010.0063
17. Nandakumar AL, Vande Voort JL, Nakonezny PA, et al. Psychometric properties of the patient health questionnaire-9 modified for major depressive disorder in adolescents. J Child Adolesc Psychopharmacol. 2019;29(1):34–40. doi:10.1089/cap.2018.0112
18. Stallwood E, Monsour A, Rodrigues C, et al. Systematic Review: the Measurement Properties of the Children’s Depression Rating Scale-Revised in Adolescents With Major Depressive Disorder. J Am Acad Child Adolesc Psychiatry. 2021;60(1):119–133. doi:10.1016/j.jaac.2020.10.009
19. Bernstein D, Fink L. Childhood Trauma Questionnaire: a retrospective self-report. The Psychological Corporation: San Antonio; 1998.
20. Baker AJ, Festinger T. Emotional abuse and emotional neglect subscales of the CTQ: associations with each other, other measures of psychological maltreatment, and demographic variables. Child Youth Serv Rev. 2011;33(11):2297–2302. doi:10.1016/j.childyouth.2011.07.018
21. Eames SF, Businelle MS, Suris A, et al. Stress moderates the effect of childhood trauma and adversity on recent drinking in treatment-seeking alcohol-dependent men. J Consult Clin Psychol. 2014;82(3):441. doi:10.1037/a0036291
22. Charlson FJ, Flaxman A, Ferrari A, Vos T, Steel Z, Whiteford H. Post-traumatic stress disorder and major depression in conflict-affected populations: an epidemiological model and predictor analysis. Global Mental Health. 2016;3.
23. Fan J, Liu W, Xia J, et al. Childhood trauma is associated with elevated anhedonia and altered core reward circuitry in major depression patients and controls. Hum Brain Mapp. 2020.
24. Cohen JR, McNeil SL, Shorey RC, Temple JR. Maltreatment subtypes, depressed mood, and anhedonia: a longitudinal study with adolescents. Psychol Trauma. 2019;11(7):704–712. doi:10.1037/tra0000418
25. Germine L, Dunn EC, McLaughlin KA, Smoller JW. Childhood Adversity Is Associated with Adult Theory of Mind and Social Affiliation, but Not Face Processing. PLoS One. 2015;10(6):e0129612. doi:10.1371/journal.pone.0129612
26. Schäfer I, Fisher HL. Childhood trauma and psychosis – what is the evidence? Dialogues Clin Neurosci. 2011;13(3):360–365.
27. Vaskinn A, Melle I, Aas M, Berg AO. Sexual abuse and physical neglect in childhood are associated with affective theory of mind in adults with schizophrenia. Schizophr Res Cogn. 2021;23:100189. doi:10.1016/j.scog.2020.100189
28. Risbrough VB, Glynn LM, Davis EP, et al. Does Anhedonia Presage Increased Risk of Posttraumatic Stress Disorder?: adolescent Anhedonia and Posttraumatic Disorders. Curr Top Behav Neurosci. 2018;38:249–265.
29. Glynn LM, Stern HS, Howland MA, et al. Measuring novel antecedents of mental illness: the Questionnaire of Unpredictability in Childhood. Neuropsychopharmacology. 2019;44(5):876–882. doi:10.1038/s41386-018-0280-9
