A digital data-driven approach was able to predict depression and allow for personalized treatment, according to study results published in Translational Psychiatry.
“There are different underlying reasons and causes for depression,” Jyoti Mishra, PhD, senior study author and assistant professor in the department of psychiatry at the University of California, San Diego, School of Medicine, said in a press release. “Simply put, current health care standards are mostly just asking people how they feel and then writing a prescription for medication. Those first-line treatments have been shown to be only mild to moderately effective in large trials.

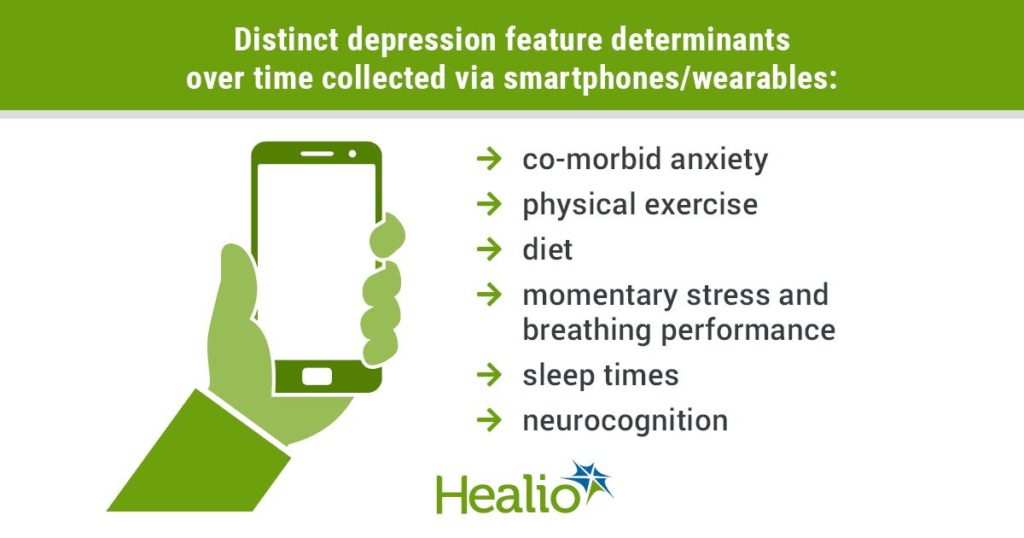
Infographic data derived from: Shah RV, et al. Transl Psychiatry. 2021;doi:10.1038/s41398-021-01445-0.
“Depression is a multifaceted illness, and we need to approach it with personalized treatment whether that be therapy with a mental health professional, more exercise or a combination of approaches,” Mishra added.
Mishra and colleagues obtained data from 14 participants with depression via smartphones applications and wearables, such as smartwatches, to measure mood and lifestyle variables, including sleep, exercise, diet and stress. They paired these with cognitive assessments and electroencephalography. Using these data, they generated individualized predictions of depressed mood over 1 month. They aimed not to compare outcomes across individuals but to model predictors of each participant’s daily fluctuations in depressed mood. Further, they used seven forms of supervised machine learning approaches, such as ensemble learning and regression-based methods, for each participant, and they verified models using fourfold nested cross-validation.
According to the researchers, there was no “one-size-fits-all strategy,” since they used a different form of machine learning model for each individual to obtain the best-fit as benchmarked by the lowest mean absolute percentage error. A composite strategy across machine learning model, or the voting regressor, performed best, on average, across participants. However, the individually selected best-fit models demonstrated significantly less error compared with the voting regressor performance across participants. The researchers used Shapley statistics for further extract top-feature predictors for each participant’s best-fit personalized model. Shapley values showed distinct depression feature determinants over time for each individual. These included co-morbid anxiety, physical exercise, diet, momentary stress and breathing performance, sleep times and neurocognition.
“Clinicians can leverage this data to understand how their patients might be feeling and better integrate medical and behavioral approaches for improving and sustaining mental health,” Mishra said. “Our study shows that we can use the technology and tools that are readily available, like cell phone apps, to collect information from individuals with or at risk for depression, without significant burden to them, and then harness that information to design personalized treatment plans.”