Source/Disclosures
Published by:
Disclosures:
Qin reports being employed by the Renal Division, Nanfang Hospital, Southern Medical University and the National Clinical Research Center for Kidney Disease and receiving grants from the National Natural Science Foundation of China. Please see the study for all other authors’ relevant financial disclosures.
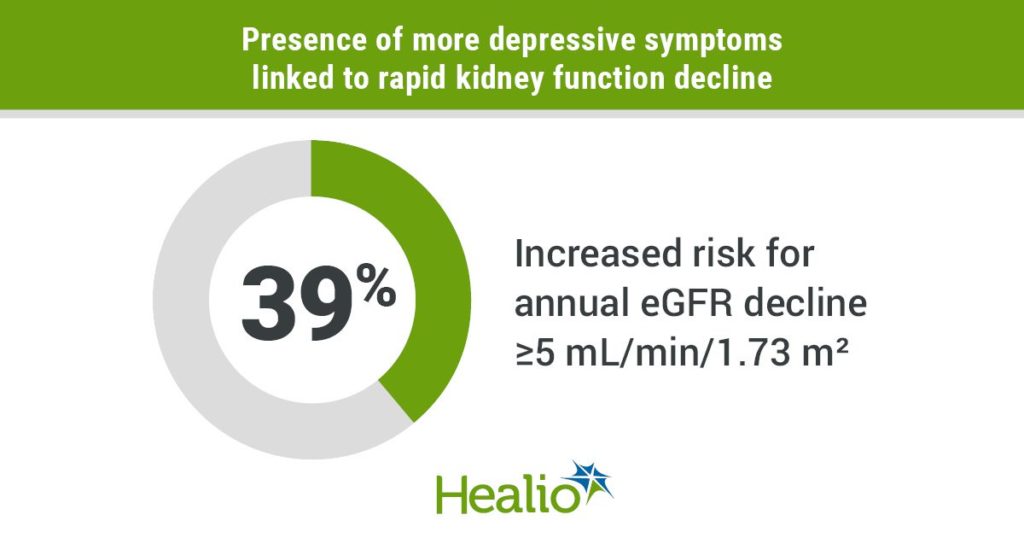
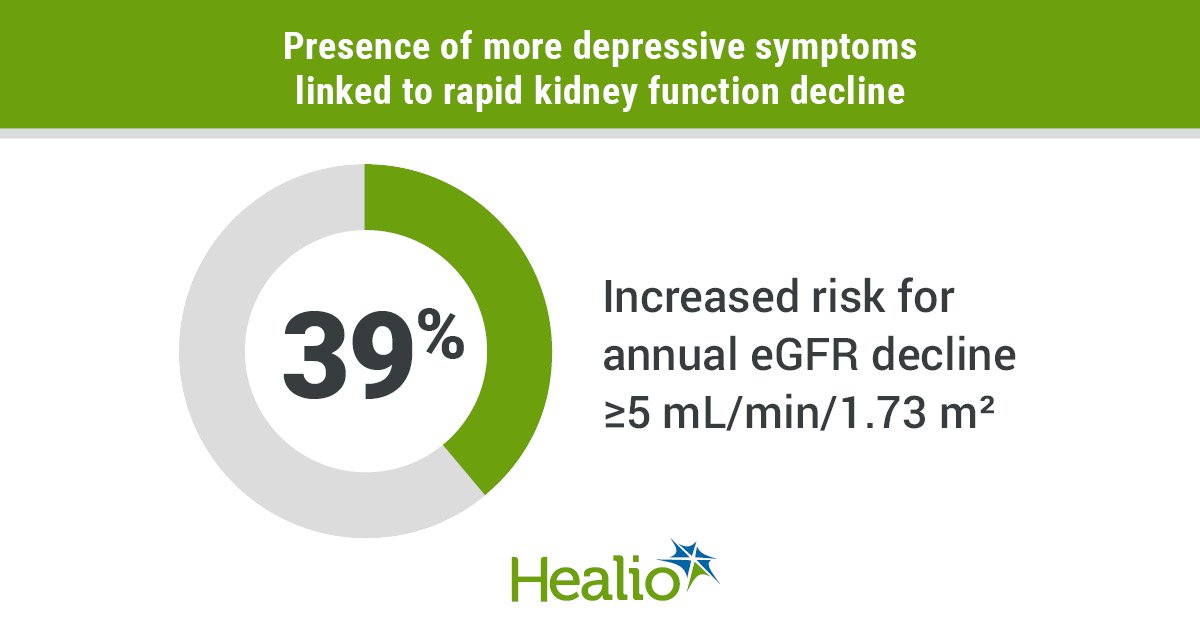
In an analysis of 4,763 adults in China with normal kidney function at baseline, the presence of high depressive symptoms was associated with a 39% increased risk for rapid decline in kidney function in a 4-year period.
The study, which was published in the Clinical Journal of the American Society of Nephrology, assessed depressive symptoms through the 10-item Center for Epidemiologic Studies Depression (CES-D) scale; through a questionnaire, participants relayed how often they experienced symptoms during the past week (scores ranged from 0 to 30; those experiencing 10 or more were considered to have “high” depressive symptoms).
Infographic content was derived from Zhang Z, et al. Clin J Am Soc Nephrol. 2021;doi:10.2215/CJN.18441120.
“[Chronic kidney disease] CKD is a leading risk factor for cardiovascular disease, kidney failure, and mortality worldwide. Therefore, the identification of more modifiable risk factors may possibly reduce the huge burden of CKD and its related complications by leading to early detection and prevention,” study co-author Xianhui Qin, MD, of Nanfang Hospital at Southern Medical University in China, said in a related press release. “While our study does not show causality, it demonstrated that high depressive symptoms were significantly associated with rapid decline in kidney function among Chinese adults with normal kidney function.”
Defining rapid kidney function decline as an annualized decline in eGFR of at least 5 mL/min/1.73 m2, Qin and colleagues found 6% of the study population experienced rapid kidney function decline in 4 years (2% developed CKD).
Depressive symptoms, kidney function decline
After adjusting for demographic, clinical and psychosocial covariates (including smoking and drinking status, marital status and education level), researchers observed a positive association between depressive symptoms and rapid decline in kidney function (per five-score increment, the adjusted odds ratio was 1.15).
In addition, 39% of the study population had a total CES-D score of 10 or more, putting them at greater risk for rapid kidney function decline compared with those with low depressive symptoms (aOR = 1.39).
“Consistently, compared with those with low depressive symptoms, participants with high depressive symptoms had lower education levels in our study,” the researchers wrote. “Participants with lower education levels may be less able to adjust their emotions and have lower selfcare awareness.”
Regarding symptoms individually, results showed four were significantly associated with rapid kidney function decline. These included being “bothered by things” (aOR = 1.16), having “trouble concentrating” (aOR = 1.17), feeling like “everything was an effort” (aOR = 1.18) or feeling lonely (aOR = 1.16). Researchers recommend additional studies be conducted to investigate the detailed mechanisms between individual symptoms and kidney function decline.
“If further confirmed, our data provide some evidence for depressive symptom screening and effective psychosocial interventions to improve the prevention of CKD,” Qin said in the release.
Patient perspective
Mary H. Wu, a kidney transplant recipient who identifies as having an American-born Chinese background and “extensive experience in health care and social services,” provided her perspective on the study in a related commentary.
“The findings of the article do not surprise me: when people are depressed, they are not as motivated to care for themselves,” she wrote. “When I was depressed, I felt paralyzed. However, I was fortunate that I was an advocate who was motivated to navigate my care at the time. I sought resources within my kidney transplant team, such as social workers.
In the United States, we are fortunate to have social workers to assist with social, emotional, and mental challenges. Mental health services need to be available when a person is in decline, not just in the final stages of kidney disease.”