Introduction
The new coronavirus disease; which emerged in China in December 2019 and which was declared a pandemic by the World Health Organization, is a new respiratory disease resulting in serious adverse consequences globally.1 The high infectiousness of severe acute respiratory syndrome coronavirus 2 (SARS COV-2) and the association of its virulence with fatal consequences resulted in the occurrence of psychological effects as anxiety disorders and depressive and obsessive–compulsive symptoms in the general population.2 The study by Vindegaard et al., reviewing 43 studies to investigate the impact of coronavirus disease 2019 (COVID-19) pandemic on mental health symptoms in the general population, has demonstrated that the pandemic not only affected mental health unfavorably but also caused an increase in the emergence of anxiety and depression symptoms.3
The new coronavirus infection affected every individual and notably expectant mothers, whose pregnancies have coincided with the pandemic. Pregnancy is a process that suppresses the immune system partially and renders women vulnerable to viral infections. The COVID-19 pandemic can cause serious unfavorable maternal and fetal consequences in pregnant women. Information about the effects of COVID-19 on pregnant women and maternal-fetal complications is growing day by day but adequate evidence has not been available yet.4 The COVID-19 pandemic naturally causes every expectant mother to develop significant fear, anxiety, and stress both about the course of pregnancy and potential impacts of the virus on their babies.5
In a study conducted in 2003, the psychological effects of the SARS outbreak on pregnant women were evaluated finding out higher anxiety levels in pregnant women.6A preliminary study has shown that the COVID-19 pandemic coinciding with the pregnancy period of women increased the rates of anxiety and depression in pregnant women.7 Again, in a multicenter study conducted by Wu et al., 4124 pregnant women in the third trimester were evaluated and it has been shown that the pandemic is a major health issue, which may potentially cause elevations in depression and anxiety rates.8 Studies in the literature report that high levels of stress in pregnant women cause many untoward consequences including preeclampsia, preterm births, stillbirths, and low Apgar scores.9–11
Getting quite out of hand and turning into a pandemic shortly; COVID-19 causes despair and hopelessness in pregnant women, as well as other individuals in society. COVID-19 has led pregnant women to implement meticulous personal hygiene habits and take more serious measures such as social restraint and isolation against infection.12 Furthermore, COVID-19 might have caused pregnant women to experience higher rates of anxiety and fear due to the risk of virus transmission to their babies.13, 14 Changes in routine work schedules in hospitals due to the pandemic and concerns on the potential of pregnant women to get infection have led to deficiencies in the pregnancy prenatal visits.12 The occurrence of stress, fear, and anxiety at higher levels than expected creates more emphasis on potential maternal, fetal, and psychiatric complications in pregnant women.14–16
No studies are available in the literature investigating the trimesters of pregnancy by their coincidence with the pandemic, examining the severity of maternal mental health disorders that might have caused by the pandemic, and investigating especially the effects of the pandemic on sleep quality. Therefore, in this study, we aimed to evaluate the level of depression and anxiety symptoms and sleep quality of pregnant women in different trimesters during COVID-19 pandemic and to investigate the effects of quarantine and lifestyle changes that come into our lives with pandemic.
Methods
Participants
This cross-sectional study included a total of 149 consecutive pregnant patients, aged between 18 and 41, who were admitted to the antenatal policlinic of Recep Tayyip Erdogan University, Faculty of Medicine, between 10 June 2020 and 10 July 2020.
Pregnant women with chronic systemic diseases, communication disorders, systemic, and obstetric complications related to pregnancy, illiterate pregnant women, pregnant women receiving treatment due to psychiatric disorders and pregnant women who disagreed to participate in the study were excluded. In addition, participants who had a history of COVID-19 infection, had suspected symptoms, or had been in close contact (any individual within 6 feet of an infected person for a total of 15 minutes or more) with someone with COVID-19 at the time of the study were not included in the study.
During the study period, 173 low-risk pregnant women at 7–39 weeks of gestation were admitted to prenatal visit. All patients underwent the comprehensive obstetric examination. Among the pregnant women, 24 patients were excluded from the study because of 18 high-risk pregnancy diagnosis, three psychiatric disease history, one history of COVID-19 infection, and two did not want to participate in the study. The sample selection was performed via the non-probabilistic sampling method. The sample size of the study was calculated as 149 with 0.230 effect size, 0.05 alpha-error value, and power (1-beta error) 0.80.
Informed consent was obtained prior to the study. The study was conducted in accordance with the ethical guidelines, including the World Medical Association (1975) Declaration of Helsinki 2008, and the legal requirements of the Ethics Committee of Recep Tayyip Erdogan University (Approval no:2020/111).
Measurements
Sociodemographic and clinical features data form
A questionnaire form was developed by the authors to collect participant information including age, marital status, education level, employment status, reproductive history, pregnancy complications, mental health history. In addition, effects of the COVID-19 pandemic on daily life activities, social relations, hygiene habits, and the quarantine history of the participants were questioned. Participants who were isolated at home for 14 days due to close contact with someone with a history of COVID-19 in past were identified as quarantined people.
Beck Depression Inventory
The 21-item multiple-question inventory to measure physical, emotional, and cognitive symptoms in depression was developed in 1961 by Beck et al.17The validity and reliability study of Beck Depression Inventory (BDI) in Turkish was carried out in 1989 by Hisli et al.18Each self-assessment item of the inventory is scored in a range from 0 to 3 points with increasing severity. The total score is calculated by adding up the item scores. The total score varies from 0 to 63 and high scores indicate increasing depression severity. In this study, the severity of depression was determined based on scale scores. Accordingly, scores of 0–10 points indicated no depression, 11–17 points indicated mild depression, 18–23 points indicated moderate depression, and 24 points and higher indicated severe depression. In the study, Cronbach’s alpha of the inventory was calculated as 0.82.19
Beck Anxiety Inventory
Beck Anxiety Inventory (BAI) is a self-rating scale developed by Beck et al. in 1988. BAI is used for determining the frequency and the severity of anxiety symptoms experienced by individuals.17BAI was adapted into the Turkish language in 1993 by Ulusoy et al.20 The reliability and the validity of BAI were confirmed to be adequate. The items of BAI are scored on a four-point Likert scale. Each of the 21 symptom categories offers four options to be selected. Each item is scored in a range from 0 to 3 points. Higher scores indicate increased anxiety severity. In this study, the scores of 0–17 points indicated low levels of anxiety, 18–24 points indicated moderate levels of anxiety, and 25 points and higher indicated high levels of anxiety. Cronbach’s alpha internal consistency score of the scale was determined as 0.93.20
Pittsburgh Sleep Quality Index
The Pittsburgh Sleep Quality Index (PSQI), developed by Buysse et al. in 1989, is a scale commonly used in psychiatry practice and clinical research.21 PSQI is validated for use in pregnant women.22The validation study of PSQI in Turkish was performed by Ağargün et al. and the Turkish version was applied to pregnant women.23 The PSQI is a 19-item self-report scale that assesses the sleep quality and sleep disturbances over the past month. The scale consists of 24 questions, of which 19 are self-report questions while five are questions to be answered by the spouse or a roommate. The 18 questions of the scale consist of seven components, which include the subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. Each component is scored in a range from 0 to 3 points. The total score received from the seven components gives the total score of the scale. The total score ranges from 0 to 21 points. A total score higher than 5 indicates “poor sleep quality”. Cronbach’s alpha value of the scale was found to be 0.79.
Statistical analysis
Kolmogorov–Smirnov (KS) test was performed and the measures of skewness-kurtosis were examined to determine the conformity of the study data to a normal distribution. As a result of these tests and examinations, it was determined that the obtained data via BDI, BAI, and PSQI did not fit a normal distribution (p < 0.001). Therefore, non-parametric tests were used in the examination of the study variables. The Mann–Whitney U test was used for comparing the means of 2 variables, the Kruskal-Wallis test was used for comparing the means of 3 or more variables and the Chi-Square test was used for examining the differences between categorical variables. In the comparisons of three or more groups, a pairwise comparison (the Bonferroni correction) was performed to identify the group creating the difference. The Linear Regression Analysis was used for conducting multiple analyses on the study variables. A bivariate correlation was performed to determine the relationship between two measurements. R-studio was used for developing the correlation matrix; Prism was used for developing other graphics, and SPSS 25.0 was used for the data analysis.
Results
Participant characteristics
The sample consisted of 149 pregnant women in the age range of 18–41 years. The mean age of the pregnant women was 30.17 ± 5.47 years. The mean body mass index (BMI) of the pregnant women was 26.00 ± 3.91. The number of pregnancies in the sample ranged from 1 to 6 with a mean of 2.03 ± 1.15. While the gestational age of the participants ranged from 7 to 39 weeks, the mean gestational week of the study participants was 22.49 ± 9.97. Of the study participants, 41.6% completed high school or higher levels of education, 60.4% were housewives, and 47.7% had equal income and expenditures. According to the week of gestation, 34.2% of the participants are in the first trimester, 30.2% are in the second trimester, and 35.6% are in the third trimester.
Depression, anxiety, and defective sleep quality scores
The relationship of the sociodemographic and clinical features of the participants with their depression, anxiety, and sleep quality levels is summarized in Table 1. When the participants were grouped according to different sociodemographic characteristics and clinical variables, it was shown that variables other than the family history of psychiatric disorder, history of quarantine, and trimester difference were not related to levels of depression, anxiety, and defective sleep (Table 1). The level of anxiety and defective sleep were statistically higher in the group with a family history of psychiatric disorder (p = 0.048, p = 0.035, respectively). The depression, anxiety, and defective sleep quality levels of the participants who were previously in the home quarantine were statistically significantly higher (p < 0.001, p < 0.001, p < 0.001, respectively). In addition, when the quarantine group was compared to the group that did not have a history of quarantine, significant differences were observed in depression, anxiety, and defective sleep quality. When evaluated according to trimester, scores of depression, anxiety, and defective sleep quality were observed to be higher in the third trimester compared to the first and second trimesters (p < 0.001, p < 0.001, p < 0.001, respectively). As for defective sleep quality, the third trimester scores were found to be higher than those found in the second and first trimesters. In addition, the second trimester scores were found to be higher than the first trimester scores (p < 0.001).
The relationship of descriptive sociodemographic and clinical variables with Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Pittsburgh Sleep Quality Index (PSQI)
| BDI | BAI | PSQI | ||||||
|---|---|---|---|---|---|---|---|---|
| Parametres | n (%) | Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | |
| Age | ≤25 years (min: 18) | 30 (20.1) | 9.30 ± 4.32 | 0.905 | 13.20 ± 6.61 | 0.666 | 6.10 ± 2.44 | 0.650 |
| 26–30 | 51 (34.2) | 10.12 ± 6.24 | 15.51 ± 9.09 | 6.80 ± 3.26 | ||||
| 31–35 | 40 (26.8) | 10.33 ± 5.76 | 15.30 ± 8.86 | 6.80 ± 3.24 | ||||
| 36 ≤ (max: 41) | 28 (18.8) | 10.64 ± 5.89 | 16.39 ± 10.10 | 7.50 ± 3.72 | ||||
| Education | Primary school and less | 21 (14.1) | 9.00 ± 4.65 | 0.651 | 15.57 ± 7.95 | 0.743 | 7.29 ± 3.61 | 0.682 |
| Secondary school graduate | 66 (44.3) | 10.77 ± 6.01 | 15.30 ± 9.10 | 6.61 ± 2.99 | ||||
| High school graduate | 7 (4.7) | 9.71 ± 7.20 | 13.14 ± 9.69 | 5.71 ± 3.73 | ||||
| University graduate | 55 (36.9) | 9.78 ± 5.43 | 15.07 ± 8.74 | 6.96 ± 3.25 | ||||
| Occupation | Housewife | 90 (60.4) | 9.80 ± 5.56 | 0.617 | 14.64 ± 8.67 | 0.775 | 6.77 ± 3.21 | 0.699 |
| Civil servant | 25 (16.8) | 9.96 ± 5.71 | 16.16 ± 9.21 | 7.08 ± 2.99 | ||||
| Blue-collar worker | 34 (22.8) | 11.03 ± 5.97 | 15.76 ± 8.85 | 6.65 ± 3.39 | ||||
| Profession of the spouse | Civil servant | 98 (65.8) | 9.99 ± 5.55 | 0.854 | 15.67 ± 9.22 | 0.358 | 6.90 ± 3.21 | 0.564 |
| Blue-collar worker | 51 (34.2) | 10.33 ± 5.93 | 14.16 ± 7.82 | 6.59 ± 3.21 | ||||
| Monthly income | Expenditure exceeds income | 48 (32.2) | 9.27 ± 5.86 | 0.215 | 13.94 ± 8.66 | 0.493 | 6.54 ± 3.20 | 0.666 |
| Income equal to expenditure | 71 (47.7) | 10.17 ± 5.33 | 15.69 ± 8.71 | 6.82 ± 3.27 | ||||
| Income exceeds expenditure | 30 (20.1) | 11.30 ± 6.06 | 15.83 ± 9.17 | 7.13 ± 3.09 | ||||
| Family type | Nuclear family | 145 (97.3) | 10.19 ± 5.72 | 0.279 | 15.19 ± 8.80 | 0.659 | 6.78 ± 3.22 | 0.648 |
| Extended | 4 (2.7) | 7.00 ± 0.82 | 14.00 ± 8.49 | 7.25 ± 2.63 | ||||
| Number of parity | 1 | 60 (40.3) | 10.18 ± 6.07 | 0.949 | 15.37 ± 9.08 | 0.706 | 6.67 ± 2.96 | 0.345 |
| 2 | 52 (34.9) | 9.94 ± 5.33 | 14.48 ± 8.75 | 6.52 ± 3.37 | ||||
| 3≤ | 37 (24.8) | 10.22 ± 5.58 | 15.76 ± 8.45 | 7.38 ± 3.35 | ||||
| Abortions | No | 123 (82.6) | 10.24 ± 5.64 | 0.443 | 15.20 ± 8.71 | 0.748 | 6.89 ± 3.16 | 0.292 |
| Yes | 26 (17.4) | 9.50 ± 5.84 | 14.92 ± 9.21 | 6.35 ± 3.39 | ||||
| Method of childbirth | No deliveries | 63 (42.3%) | 10.27 ± 6.15 | 0.833 | 15.41 ± 9.17 | 0.989 | 6.68 ± 2.97 | 0.984 |
| Normal vaginal | 45 (30.2) | 10.29 ± 5.43 | 15.07 ± 8.97 | 7.02 ± 3.53 | ||||
| Cesarean delivery | 41 (27.5) | 9.66 ± 5.22 | 14.85 ± 8.10 | 6.71 ± 3.23 | ||||
| Gestational week | First trimester | 51 (34.2) | 7.08 ± 4.03 | <0.001a | 9.33 ± 5.27 | <0.001a | 4.02 ± 1.09 | <0.001a |
| Secondary trimester | 45 (30.2) | 7.69 ± 3.38 | 11.16 ± 4.85 | 6.22 ± 2.09 | ||||
| Third trimester | 53 (35.6) | 15.08 ± 5.17 | 24.15 ± 6.53 | 9.94 ± 2.52 | ||||
| Psychiatric disorder in family history | Yes | 7 (4.7) | 13.29 ± 5.59 | 0.093 | 20.86 ± 6.91 | 0.048 | 9.29 ± 2.87 | 0.035 |
| No | 142 (95.3) | 9.95 ± 5.64 | 14.87 ± 8.77 | 6.67 ± 3.17 | ||||
| Quarantine | Yes | 75 (50.3) | 11.72 ± 6.35 | 0.002 | 17.84 ± 9.93 | 0.002 | 7.64 ± 3.49 | 0.002 |
| No | 74 (49.7) | 8.47 ± 4.34 | 12.43 ± 6.40 | 5.93 ± 2.62 | ||||
| Total | 149 (100.0) | 10.11 ± 5.663 | 15.15 ± 8.77 | 6.79 ± 3.20 | ||||
- Note: p < 0.05 was accepted to be statistically significant. Statistically significant p values are written in bold.
- a
The factor resulting in the significance is the higher third trimester scores compared to the first and second trimester scores for depression and anxiety; (p < 0.001) score means that higher sleep quality results in three trimester scores compared to the two and one trimesters; also, the two trimester scores is higher than the one trimester score (pairwise comparison [Bonferroni correction]).
As shown in Table 2, when participants were grouped according to trimester, sociodemographic, and clinical characters were shown to be similar in the three groups.
Comparison of sociodemographic and clinical characters of pregnant women in groups formed according to trimester
| First trimester | Second trimester | Third trimester | ||||
|---|---|---|---|---|---|---|
| Parametres | n (%) | n (%) | n (%) | n (%) | p | |
| Age | ≤25 years (min: 18) | 30 (20.1) | 12 (23.5) | 7 (15.6) | 11 (20.8) | 0.572 |
| 26–30 | 51 (34.2) | 14 (27.5) | 17 (37.8) | 20 (37.7) | ||
| 31–35 | 40 (26.8) | 17 (33.3) | 13 (28.9) | 10 (18.9) | ||
| 36 ≤ (max: 41) | 28 (18.8) | 8 (15.7) | 8 (17.8) | 12 (22.6) | ||
| Education | Primary school and less | 21 (14.1) | 9 (17.6) | 5 (11.1) | 7 (13.2) | 0.416 |
| Secondary school graduate | 66 (44.3) | 26 (51.0) | 16 (35.6) | 24 (45.3) | ||
| High school graduate | 7 (4.7) | 1 (2.0) | 4 (8.9) | 2 (3.8) | ||
| University graduate | 55 (36.9) | 15 (29.4) | 20 (44.4) | 20 (37.7) | ||
| Occupation | Housewife | 90 (60.4) | 32 (62.7) | 27 (60.0) | 31 (58.5) | 0.801 |
| Civil servant | 25 (16.8) | 6 (11.8) | 9 (20.0) | 10 (18.9) | ||
| Blue-collar worker | 34 (22.8) | 13 (25.5) | 9 (20.0) | 12 (22.6) | ||
| Profession of the spouse | Civil servant | 98 (65.8) | 30 (58.8) | 31 (68.9) | 37 (69.8) | 0.438 |
| Blue-collar worker | 51 (34.2) | 21 (41.2) | 14 (31.1) | 16 (30.2) | ||
| Monthly income | Expenditure exceeds income | 48 (32.2) | 20 (39.2) | 13 (28.9) | 15 (28.3) | 0.574 |
| Income equal to expenditure | 71 (47.7) | 24 (47.1) | 21 (46.7) | 26 (49.1) | ||
| Income exceeds expenditure | 30 (20.1) | 7 (13.7) | 11 (24.4) | 12 (22.6) | ||
| Family type | Nuclear family | 145 (97.3) | 51 (100.0) | 43 (95.6) | 51 (96.2) | 0.179 |
| Extended | 4 (2.7) | 0 (0.0) | 2 (4.4) | 2 (3.8) | ||
| Number of parity | 1 | 60 (40.3) | 20 (39.2) | 17 (37.8) | 23 (43.4) | 0.674 |
| 2 | 52 (34.9) | 21 (41.2) | 14 (31.1) | 17 (32.1) | ||
| 3≤ | 37 (24.8) | 10 (19.6) | 14 (31.1) | 13 (24.5) | ||
| Abortions | No | 123 (82.6) | 40 (78.4) | 39 (86.7) | 44 (83.0) | 0.565 |
| Yes | 26 (17.4) | 11 (21.6) | 6 (13.3) | 9 (17.0) | ||
| Method of childbirth | No deliveries | 63 (42.3%) | 20 (39.2) | 18 (40.0) | 23 (47.2) | 0.335 |
| Normal vaginal | 45 (30.2) | 18 (35.3) | 10 (22.2) | 17 (32.1) | ||
| Cesarean delivery | 41 (27.5) | 13 (25.5) | 17 (37.8) | 13 (20.8) | ||
| Psychiatric disorder in the family history | Yes | 7 (4.7) | 1 (2.0) | 1 (2.2) | 5 (9.4) | 0.141 |
| No | 142 (95.3) | 50 (98.0) | 44 (97.8) | 48 (90.6) | ||
- Note: p < 0.05 was accepted to be statistically significant.
The relationship of the effects of the COVID-19 pandemic on daily life activities, social relations, hygiene habits of the participants with their depression, anxiety, and sleep quality levels is summarized in Table 3. As shown in Table 3, we found that pregnant women who stated that they were affected by these lifestyle changes had higher levels of depression, anxiety, and defective sleep quality.
The relationship of the effects of the COVID-19 pandemic on daily life activities, social relations, hygiene habits with Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Pittsburgh Sleep Quality Index (PSQI)
| Question | n (%) | BDI | BAI | PSQI | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | |||
| Increase in cleaning/hygiene efforts | Yes | 127 (85.2) | 10.72 ± 5.77 | <0.001 | 16.17 ± 8.97 | <0.001 | 7.13 ± 3.22 | <0.001 |
| No | 22 (14.8) | 6.59 ± 3.38 | 9.27 ± 4.09 | 4.82 ± 2.24 | ||||
| Not going out, staying home longer, not being able to enter public places | Yes | 101 (67.8) | 11.63 ± 5.93 | <0.001 | 17.50 ± 9.08 | <0.001 | 7.66 ± 3.23 | <0.001 |
| No | 48 (32.2) | 6.90 ± 3.27 | 10.21 ± 5.45 | 4.96 ± 2.24 | ||||
| Less contact with other people (handshaking, hugging…) | Yes | 106 (71.1) | 11.28 ± 6.08 | <0.001 | 17.15 ± 9.26 | <0.001 | 7.37 ± 3.29 | <0.001 |
| No | 43 (28.9) | 7.21 ± 2.92 | 10.23 ± 4.66 | 5.37 ± 2.47 | ||||
| Excessive anxiety, fear, avoidance of coughing or sick-looking people other | Yes | 78 (52.3) | 11.51 ± 6.50 | 0.001 | 17.19 ± 10.23 | 0.002 | 7.28 ± 3.62 | 0.046 |
| No | 71 (47.7) | 8.56 ± 4.09 | 12.92 ± 6.15 | 6.25 ± 2.58 | ||||
| Total | 149 (100.0) | 10.11 ± 5.663 | 15.15 ± 8.77 | 6.79 ± 3.20 | ||||
- Note: p < 0.05 was accepted to be statistically significant. Statistically significant p values are written in bold.
In the correlation analysis carried out, while the depression, anxiety, and defective sleep quality scores were not statistically significantly correlated with age, BMI, and the number of pregnancies, a significant correlation was observed with the gestational week. As shown in Figure 1, a moderately significant positive correlation was observed between the gestational week and depression. In addition, the gestational week was highly significantly and positively correlated with the defective sleep quality and anxiety scores. There was a positive correlation between the defective sleep quality scores and not only with the depression scores but also with the anxiety scores (Figure 1).
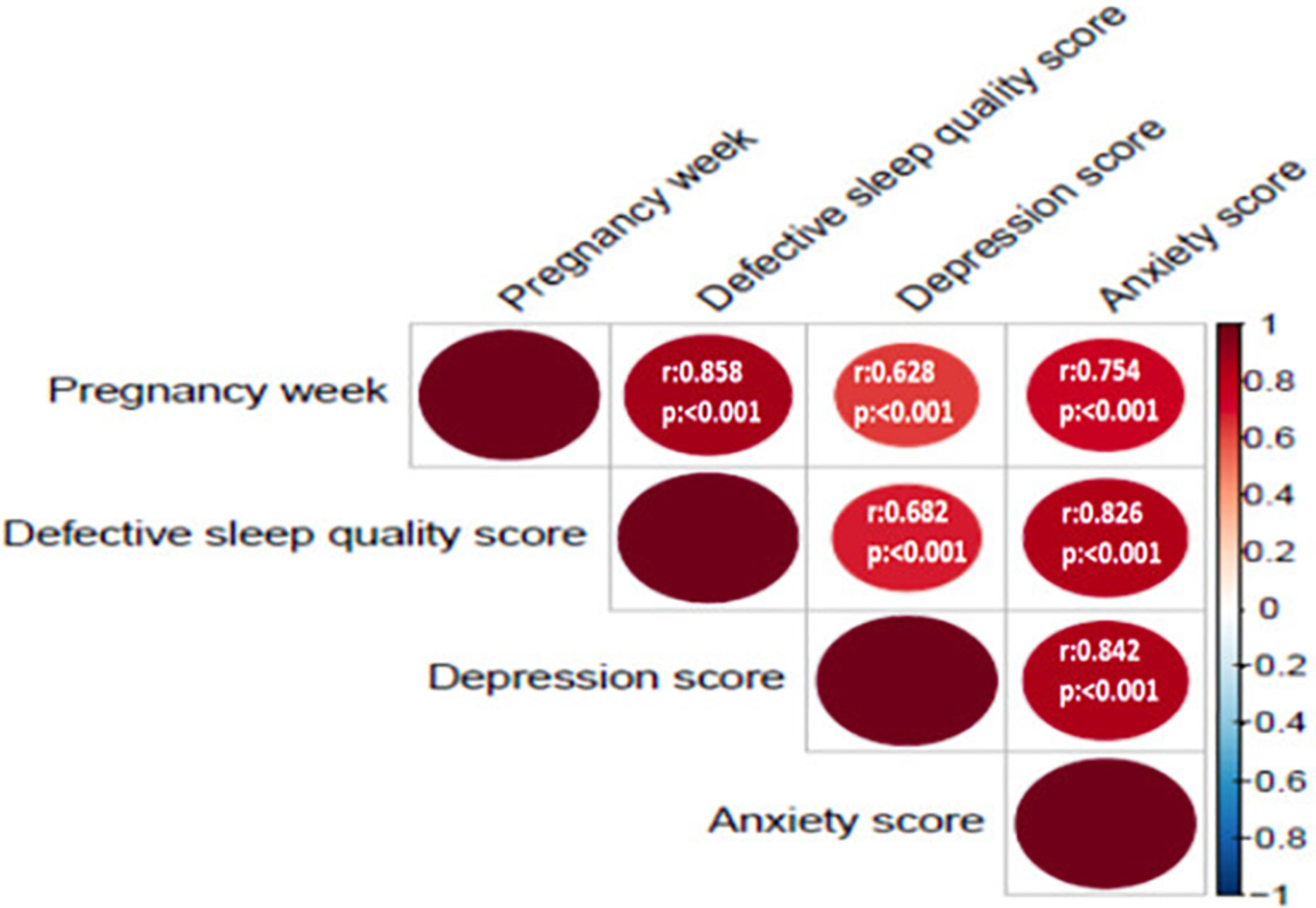
Correlation matrix showing the correlation of the gestational week with the scores of sleep quality, depression, and anxiety
In Table 4, the percentages of pregnant women affected by changes in daily living activities, social relationships, and hygiene habits during the COVID-19 pandemic were compared among the groups formed according to trimester. Accordingly, the percentages of being affected by on daily life activities, social relations, hygiene habits were statistically significantly higher in pregnant women in the last trimester compared to the first and second trimester.
Comparison of the percentages of pregnant women affected by changes in daily living activities, social relationships, and hygiene
| 1st trimester | 2nd trimester | 3rd trimester | p | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Question 1 | 38 (74.5) | 38 (84.4) | 51 (96.2) | 0.008 |
| Increase in cleaning/hygiene efforts | ||||
| Question 2 | 26 (51.0) | 27 (60.0) | 48 (90.6) | <0.001 |
| Not going out, staying home longer, not being able to enter public places | ||||
| Question 3 | 31 (60.8) | 27 (60.0) | 48 (90.6) | <0.001 |
| Less contact with other people (handshaking, hugging…) | ||||
| Question 4 | 23 (45.1) | 20 (44.4) | 35 (66.0) | 0.044 |
| Excessive anxiety, fear, avoidance of coughing or sick-looking people other |
- Note: n indicates the number of participants who answered yes to the question.
Discussion
Our study is the first descriptive study evaluating the effect of the life-threatening COVID-19 pandemic on the maternal mental health and sleep quality in each trimester in pregnant women. In our study, we observed that the scores of depression, anxiety, and defective sleep quality increased significantly as the gestational week progressed. The BDI, BAI, and PSQI scores were found significantly higher especially in the third trimester compared to the first and second trimesters. Another major finding in our study is that history of home quarantine due to the pandemic caused significant increases in the scores of depression, anxiety, defective sleep quality in pregnant women. In addition, we found that the percentages of being affected by on daily life activities, social relations, hygiene habits were higher in pregnant women in the third trimester compared to the first and second trimester and pregnant women who stated that they were affected by these lifestyle changes and followed the rules had higher levels of depression, anxiety, and defective sleep quality.
A study in the literature has examined the factors acting on stress and anxiety that may arise due to COVID-19 pandemic in pregnant women and shown that a variety of sociodemographic data can cause changes in anxiety levels.24 It was shown that the anxiety and stress levels were higher especially in subgroups with low income and low education levels. However, in our study, sociodemographic data did not cause a statistically significant difference in the severity of depression and anxiety and in the defective sleep quality in pregnant women. This finding might have resulted from the fact that the Ministry of Health has provided safe access to health services for every individual in the society and provided information about the pregnancy prenatal visits regularly.
A multicenter comparative study, which investigated perinatal depression and anxiety in the third trimester after the declaration of the COVID-19 pandemic in China, found significant elevations in the rates of depression and anxiety in pregnant women in the third trimester of pregnancy after the announcement of the pandemic.8 In our study carried out after the pandemic declaration, the depression and anxiety rates were found high in each trimester of pregnancy but statistically significant differences were observed across the trimesters. There was a significant increase in the depression and anxiety scores in our study, especially in the third trimester compared to the first and second trimesters. With the progression of the gestational week, the bond between the mother and the fetus may be stronger because of both hormonal and emotional changes in the pregnant woman. In our study, as shown in Table 2, there is no difference in terms of sociodemographic and clinical characters of pregnant women in groups formed according to trimesters. However, as the trimester increases, it is observed that daily living activities, social habits, and hygiene habits of pregnant women are affected in relation to the COVID-19 pandemic (Table 4). The increases in the severity of fear and anxiety due to the pandemic may be due to the advanced gestational age.
Of the measures taken during the COVID-19 pandemic, the effects of quarantine on maternal psychiatric symptoms in the postpartum period were investigated in a study from Italy, where seriously untoward consequences of the pandemic occurred.25 The study found out higher scores of anxiety, depression, and anhedonia during the postpartum period in the quarantine group compared to the control group. Depending on the psychological impact of quarantine, individuals may experience a variety of mood changes. Being in quarantine can cause fear, anxiety, and stress; as well as anger, nervousness, and feelings of guilt.26 Similar to the psychological effects of quarantine reported in the literature; in our study, we found higher scores of depression, anxiety, and defective sleep quality in pregnant women, who had history of home quarantine.
When we performed a literature review, we have observed that information is available, and the number of respective studies is increasing about the changes in maternal mental health due to the COVID-19 pandemic. However, we have not found any data about the effects of COVID-19 pandemic on sleep quality in pregnant women in each trimester in the literature. We think that our study is the first one investigating this subject matter. In a general population-based study conducted in Italy with the participation of 1515 people, psychological and social effects of COVID-19 were examined. In that study, 42.2% of the participants had reported sleep problems and, of those, 62.7% had mild insomnia and 16.3% had clinical insomnia. Furthermore, the multivariate modeling of this study revealed a positive relationship of the female gender with both anxiety and sleep disorders.27 The effects and risk factors of the COVID-19 pandemic on mental health were evaluated with associated risk factors in a large-scale general population-based prevalence study, in which 52.12% of the 56 932 participants were women. That study found out that the pandemic caused a significant increase in the rates of depression and anxiety, as well as of insomnia, in the general population.28 Still in that study, it was shown that the sleep disorder scores increased in the quarantine group. In our study on pregnant women, we detected sleep disorder in all patients during the pandemic period, especially in the third trimester compared to the first and the second. We observed high scores of defective sleep quality. We observed statistically significant higher sleep disorder scores in the pregnant women who had history of home quarantine compared to the group of pregnant women, who had not. Our study shows that the changing daily life activities, social relations, and hygiene habits of pregnant women with the pandemic are also statistically related to defective sleep quality, as shown in Table 3. Furthermore, we found that defective sleep quality scores increased in positive correlation with the depression and anxiety scores in our study. We think that the pandemic may not cause isolated sleep disorders in pregnant women and that sleep disorders occurring in pregnant women should be evaluated in combination with the unfavorable effects of the COVID-19 pandemic on mental health because clinical sleep disturbances can cause maternal–fetal complications. A systematic review and meta-analysis have shown that elevated levels of proinflammatory cytokines caused by sleep disorder in pregnant women and endothelial damage originating from oxidative stress can lead to obstetric complications and are associated with poor perinatal outcomes.29, 30
Studies in the literature report that psychiatric symptoms and sleep disorders are more common in individuals with a family history of a psychiatric disorder.31, 32 We have found that the scores of anxiety, which is a psychiatric symptom, were higher with a weak statistical effect size in the group with a family history of a psychiatric disorder in our study. The low number of the study population might have caused the weak effect size.
Pregnant women, like all individuals in the population, were affected by the COVID-19 pandemic parallel to the spread of the pandemic globally. Also, pregnant women are more prone to risks and are more vulnerable as they are expecting a child. The results of our study show that the COVID-19 pandemic caused significantly higher depression, anxiety, and defective sleep scores in pregnant women. Furthermore, a close pregnancy prenatal visit program and a multidisciplinary approach for depression, anxiety, and sleep disorders may be a prudent approach during the pandemic as the scores of depression, anxiety, and sleep disorders show increases in later trimesters. Depression, anxiety, and sleep disturbances that occur during pregnancy can lead to serious perinatal and psychiatric complications. Because especially the third trimester scores were higher compared to the two other trimesters in our study, these patients might need close follow-up programs and a multidisciplinary approach for postpartum depression, post-traumatic stress disorder, and insomnia in the postpartum period. Besides the risk of viral contamination during the COVID-19 pandemic, disorders in maternal mental health and sleep disturbances in the perinatal period may be other major foci of attention that we need to evaluate.
Since our study shows that there may be an increase in the severity of the mental health symptoms and sleep disorder scores especially with the progression of gestational weeks, we think that future larger-scale multicenter studies will shed further light on this subject matter. Because our study is the first in investigating the defective sleep quality in pregnant women during the pandemic between the trimesters, we think that it will be a pioneering study for more detailed research about sleep disorders.
However, the inclusion of only the pregnant women, who could attend the pregnancy prenatal visits into the study during the pandemic, and the single-center study design prevent the generalization of the results of this cross-sectional study. Also, the lack of the evaluation the study patients for depression, anxiety, and sleep disturbances in the period before the pregnancy and in the postpartum period is another limitation of our study. Another limitation is that during the time the study was conducted, the pandemic still continued in our country, so the study was designed as cross-sectional, data could not be compared with the control group as in case control statistical method. For this reason, it may not have been clearly shown whether the results of depression, anxiety scores, and sleep quality of pregnant women depend on the effect of the COVID-19 pandemic. We think that the studies to be carried out with the case control method to be designed when the COVID-19 pandemic is over will yield stronger results. As a result, during the COVID-19 pandemic process, we found that there was an increasing worsening in the symptoms of depression and anxiety and defective sleep quality of pregnant women as the week of gestation progressed. We have shown that anxiety, depression, and defective sleep quality are more common in pregnant women affected by lifestyle changes (Increase in cleaning, not going out, less contact with other people, fear of getting sick, etc.) that are increasingly included in our lives, especially with pandemic conditions, and this is more common in pregnant women within advancing trimesters (Table 4). In other words, the pandemic affects women in the third trimester at a higher rate in terms of both mental health symptoms and sleep quality. It may be necessary to be more careful in detecting perinatal and psychiatric complications that may occur both during pregnancy and in the postpartum period. We think that potential unfavorable effects of COVID-19 can be prevented and treated by practicing an active, multidisciplinary, and close prenatal and postnatal visit program during the pandemic. However, as the COVID-19 pandemic is ongoing, our data need to be confirmed and investigated in future more extensive population studies.
Conflict of Interest
No potential conflict of interest was reported by the authors.