According to the World Health Organization, 20 percent of children and adolescents experience mental illnesses, with neuropsychiatric conditions being the most common disability in teenagers.1 Despite this, mental health remains relatively neglected in the pediatric population. The U.S. Department of Health and Human Services has recognized depression as a public health concern and a leading cause of both injury and disease.2 The prevalence of these mental health conditions increases in the presence of a chronic condition or disability, such as hearing loss.

Shutterstock/Kataryna Lanskaya, hearing loss, depression, mental health.
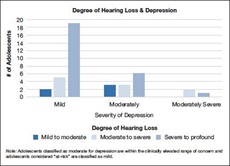
Adolescent scores on PHQ-8 by the degree of hearing loss, hearing loss, depression, mental health.
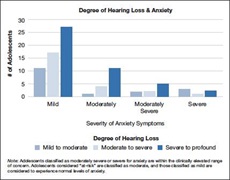
Adolescent scores on GAD-7 by the degree of hearing loss, hearing loss, depression, mental health
Depression and anxiety are among the most common mental health conditions experienced in adolescence and adulthood.3 Depression is characterized by persistent feelings of sadness, diminished interest in activities, fatigue, feelings of worthlessness, and changes in eating and sleeping patterns.4 Childhood depression is infrequent; however, its prevalence increases in adolescence and tends to be more common in women.3 Anxiety is characterized as persistent feelings of worry that are difficult to control and results in irritability, sleep disturbance, or difficulty concentrating.4 The most common and broad diagnosis is a generalized anxiety disorder, which is often identified in later adolescence.
Research in the area of mental health and hearing loss is generally not investigated or remains rather limited. The existing published studies have demonstrated variabilities within the hearing loss population, with some studies reporting that nearly 25-38 percent of children experience symptoms of sadness, worry, and social withdrawal, while other studies report no difference in the hearing loss population whatsoever.3,5
Identification and intervention of mental health conditions, such as depression and anxiety are crucial, as they are linked to long-term outcomes and compliance to treatment. For the hearing loss population, mental health intervention can impact device use and involvement in rehabilitative programs, which can affect or predict the quality of life and/or speech and language outcomes.6 Mental health can also negatively affect school performance and productivity.7
Our study implemented as a standard of care a universal screening protocol for depression and anxiety in adolescents serviced in an otology/audiology practice. The study aimed to estimate the prevalence of depression and anxiety in adolescents with hearing loss.
STUDY METHODS
We recruited 104 adolescents ages 12-18 years from an otology clinic. Given that we wanted to focus on the association between hearing loss and mental health, patients with normal hearing were excluded from the study. The final sample was 92 adolescents with an average age of 14 years (SD=1.82) of which 58.7 percent self-reported as Hispanic, and 62 percent had bilateral hearing loss. Patients completed a mental health screener once per year as part of their standard clinical care. Patients also completed demographic information and a medical record review was completed to gather information on their type and degree of hearing loss. Patients independently completed the screener on an iPad. If patients scored above the clinical cutoff, a brief consultation was conducted by the family support team with the adolescent and their parent, and referrals were provided.
The measures used in the screener consisted of the Patient Health Questionnaire (PHQ-85) and the Generalized Anxiety Disorder questionnaire (GAD-78). These measures assess depression and anxiety symptoms, respectively. Both measures are widely used, available in multiple languages, and are considered reliable and valid. Further, patients were asked “If you are experiencing any of the problems on this form (questions above), how difficult have these problems made it for you to do your work/school, take care of things at home or get along with other people?” Patients then indicated their impairment on a range from “not at all difficult” to “extremely difficult.”
RESULTS & HIGHLIGHTS
Twenty-five percent of adolescents scored above the clinical cut-off on at least one of the measures and nine percent scored in the elevated range on both measures. More importantly, 30 percent of patients scored in the at-risk range for depression and 21 percent for anxiety. Our results illustrate the need for prevention work to reduce symptoms of depression or anxiety before they develop into psychological disorders. Older adolescents reported more symptoms of depression compared to younger children (r =.232, p =.026). In addition, adolescents with bilateral sensorineural hearing loss were more likely to report elevated symptoms of depression (18%), followed by unilateral hearing loss (15%), bilateral conductive hearing loss (18%), and bilateral mixed hearing loss (33%). Similarly, adolescents with bilateral sensorineural hearing loss (18%) reported more symptoms of anxiety, followed by unilateral hearing loss (25%). In general, adolescents scoring above the cut-off on the depression measure had severe to profound hearing loss, followed by moderate to severe, and mild to moderate (Fig. 1). Similarly, on the anxiety measure, we found that adolescents with severe to profound hearing had a higher rate of clinically elevated anxiety scores, followed by mild to moderate, and moderate to severe (Fig. 2). Lastly, no significant associations were found between mental health symptoms and type of hearing device. However, the majority of adolescents scoring above the clinical cut-off wore hearing aids followed by cochlear implants, or no device.
CLINICAL APPLICATION & RECOMMENDATIONS
Our study highlighted the need for mental health screening as part of otology and audiology practices. Moreover, it showed that implementation of a screener is both feasible and warranted given the elevated concerns reported by adolescents with hearing loss. Given these data, it is recommended that mental health screeners be an integral part of annual visits for patients with hearing loss. The mental health screener takes less than five minutes to complete and can be easily administered by office staff, audiology assistants, students, or nurses. Often patients and/or parents will have enough time to finish the screener while waiting to see the audiologist or otolaryngologist. The medical visit can begin with a quick review of the screener results and a discussion with the patient and/or parents. If the results suggest the patient is at risk for anxiety or depression, direct referrals can be made to the team psychologist or social worker to further discuss the screener results. In cases where these providers are not readily available, the physician or audiologist may provide the family with local community referrals for mental health services.
While some audiology and otology clinics may be reluctant to administer a mental health screener due to reimbursement and clinic efficiency concerns, the benefits of addressing depression and anxiety in adolescents with hearing loss outweighs these clinical profitability concerns. Children with depression and/or anxiety are seven times more likely to have accrued more than two weeks of school absences7 and are three times more likely to be non-compliant with medical treatment recommendations.2 As such, untreated mental health issues are likely to contribute to decreased wear time of hearing devices (hearing aids, cochlear implants, and acoustic implants) which, as a result, will negatively affect communication abilities, quality of life, speech understanding, and social interactions.
In conclusion, with increasing rates of depression and anxiety in the world and the hearing loss population being disproportionately at-risk, integration of mental health screening is urgently needed to both identify those who require psychological support and to link them to appropriate intervention to reduce long-term impact on the quality of life and mental health functioning. See original article10 for further information.

