Source/Disclosures
Source:
Healio Interview
Disclosures:
Patterson reports no relevant financial disclosures.
May is Maternal Mental Health Awareness Month, meant to raise awareness of maternal mental health problems during and after pregnancy, including postpartum depression.
The U.S. Preventive Services Task Force, American College of Obstetricians and Gynecologists and AAP all recommend screening for depression in postpartum women.
Reference: Bauman BL, et al. MMWR. 2020;doi:10.15585/mmwr.mm6919a2.
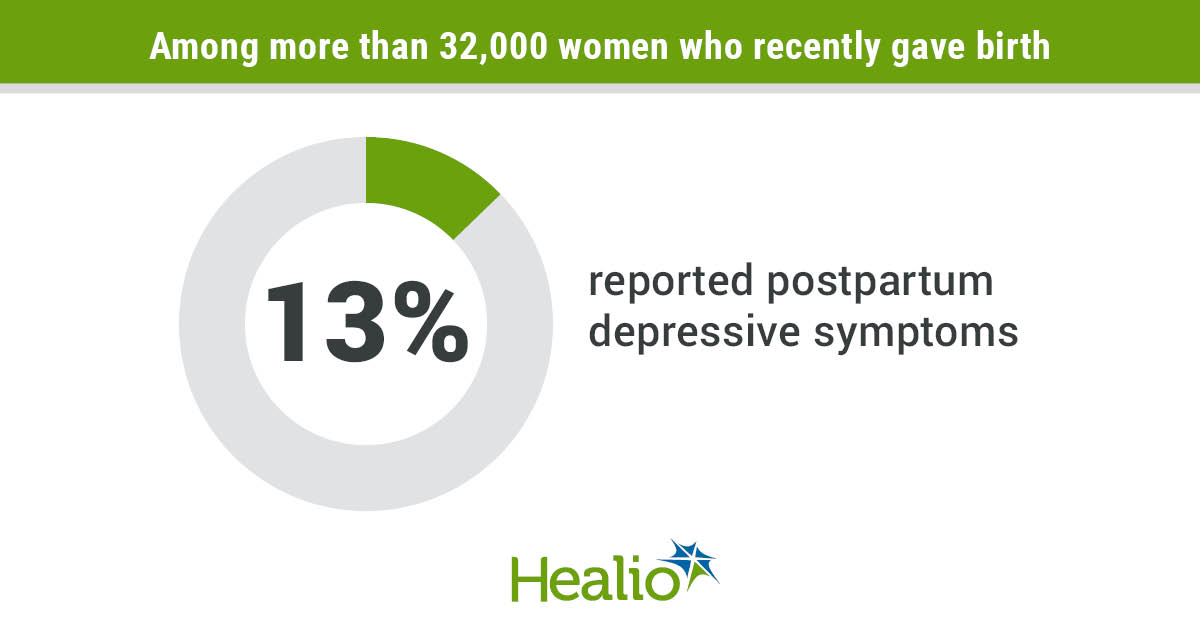
According to data published in MMWR, 13% of 32,659 women with a recent live birth reported depressive symptoms during the postpartum period, and 12.4% of those women said they were never asked about depression during a postpartum visit.

Riah Patterson
Healio Primary Care asked Riah Patterson, MD, an assistant professor at UNC Chapel Hill and medical director of its perinatal psychiatry in-patient unit, to discuss symptoms of postpartum depression that some physicians may miss and effective approaches to treatment.
Healio Primary Care: What are some symptoms of postpartum depression that primary care physicians might overlook?
Patterson: Irritability, elevated anxiety, insomnia, obsessional and intrusive thoughts, poor attachment and difficulty bonding with the infant. All of these, to some degree, can be normal postpartum experiences and feelings. Yet if they impair daily function, they can be a sign of perinatal or postpartum mood and anxiety disorder.
Healio Primary Care: Why do you think physicians are hesitant to ask their patients about postpartum depression?
Patterson: MDs often feel comfortable addressing things they know most about and feel confident in treating. Training on women’s mental health is relatively new and still could be improved. It can be hard to differentiate between the expected exhaustion and anxiety of being postpartum, baby blues and perinatal/postpartum mood or anxiety disorders.
Perinatal mental health is a nuanced field that can be difficult to talk about, holds stigma, requires consideration of patient expectations, while acknowledging that many physiological changes are taking place. Physicians may have the best intentions but due to time constraints and inexperience, some may not feel comfortable asking about perinatal/postpartum mood or anxiety disorders.
Healio Primary Care: In 2019, the FDA approved Zulresso (brexanalone, Sage Therapeutics), an IV treatment for postpartum depression in adult women. What results have you seen so far with the drug?
Patterson: This is the first FDA-approved treatment for postpartum depression. It is a 60- hour infusion, and we have had success with this treatment at UNC. Many of our patients feel relief during the infusion, and we are now gathering longer-term data post infusion. Our patients have given positive feedback about the treatment, and many have remained in remission since the infusion.
Healio Primary Care: What other treatments or interventions do you recommend for women with postpartum depression? How effective are they?
Patterson: The best approach is going to be patient specific. Some women respond very well to psychotherapy, while others with more moderate or severe symptoms may benefit from the combination of therapy and standard antidepressants. Still, some will need more tailored care with the Zulresso infusion.
Healio Primary Care: When should a woman experiencing postpartum depression be referred to a psychiatrist or psychologist?
Patterson: I would recommend referral to a perinatal mental health specialist if there are diagnostic concerns, lots of psychiatric comorbidity, little response to standards of care, and if there are safety concerns, such as suicidality or psychosis.
References:
Bauman BL, et al. MMWR. 2020;doi:10.15585/mmwr.mm6919a2.
Postpartum Support Virginia. Celebrate maternal mental health month in May! https://postpartumva.org/maternalmentalhealthmonth/. Accessed May 3, 2021.
UTHealth. Maternal mental health awareness month. https://med.uth.edu/psychiatry/2020/05/27/maternal-mental-health-awareness-month/. Accessed May 3, 2021.